
[cmamad id=”18631″ align=”center” tabid=”display-desktop” mobid=”display-desktop” stg=””]
You can prevent or fix heart disease… But they don’t tell men about this… Here is the full story…
——-Important Message——
My penis got bigger… And here’s how
Not long ago, I realized my balls had shrunk and they were not as heavy… And it seemed that I never had an erection anymore, even when I woke up.
My doctor said, “That happened to me too…” and didn’t have any ideas for me.
But it turns out that my problem was a physical one that is never diagnosed…
I had this problem for YEARS and saw seven doctors… Out of the seven doctors, not ONE ever diagnosed it or suggested anything constructive…
And then I discovered that 22% of men have this same problem – and their doctors don’t know it!
(Other than one doctor who said he could cut it open and insert penile implants. No thanks!)

————-
Why is the American Medical Association hiding this?
Scientists figured this out nearly 30 years ago, but the medical industry ignores it because of the implications that follow from it.
It shows there is actually a benefit to high cholesterol (otherwise known as familial hypercholesterolemia).
If that is true (and I think it is), it shows us how to prevent virtually all heart disease – easily.
But having an entire country without cardiovascular disease is not on the AMA’s wish list: Cardiology is their second greatest revenue source behind cancer.
And thousands of distributors and suppliers make millions from producing related drugs and supplies.
The status quo always involves a certain degree of inertia, powerfully resisting change.
If everybody knew the truth, hundreds of thousands of AMA members and pharmacologists would be out billions of dollars every year.
Distributors would need to find other things to distribute.
And realtors would have to find some other use for the Cleveland Clinic – perhaps they could renovate it into a shopping mall.
[cmamad id=”18632″ align=”center” tabid=”display-desktop” mobid=”display-desktop” stg=””]
Above all – the AMA can’t admit they’ve made a significant error until after 50 years have elapsed…
They must not “lose the trust of the public.”
The substantial evidence for lipoprotein(a) (Lp(a)) involvement is important to consider because we can do a lot of harm if we focus on the non-causal parameters (which we do right now).
You know, the red herrings such as LDL (low-density lipoproteins or “bad” cholesterol).
We have so many significant food dangers to worry about these days (aluminum, iron, omega-6 fatty acids)…
So we don’t actually need to be distracted by worrying about saturated fats and cholesterol – both of which are practically innocuous to consume.
“We have found the high-cholesterol patients survive about as long as their unaffected relatives. Our finding is that familial high cholesterol is compatible with survival into the sixth, seventh, and eighth decades…”
And this knowledge leads to a very simple cure and prevention…
So simple that it is totally unprofitable for the AMA and the pharmaceutical industries…
And that’s why we have this intentional ignorance and suppression.
Lp(a) is similar to LDL, but it has a unique protein called apo(a).
This protein does not correlate with any of the other “risk factors” and only a few species of mammals have it.
Perhaps this is why most mammals, such as dogs and rats, can only end up with cardiovascular disease by using the most dedicated lab methods.
The best models for cardiovascular disease are primates and pigs. This is probably because primates can’t synthesize their own vitamin C and pigs only have a diminished capacity to do that – about threefold less than dogs.
We mammals need vitamin C so our bodies can crosslink collagen strands.
Our bodies do this by forming hydroxyproline groups on them.
Without this one essential vitamin, the extracellular matrix will eventually break down. And we all heard about scurvy in history class…
Scurvy is characterized by spontaneous bruising, slow wound healing, and increased synthesis of lipoprotein(a).
Since we need vitamin C to physically crosslink collagen, it makes sense that it also signals for its synthesis more than anything else does – about fourfold.
Lp(a) binds to lysine groups, but not to hydroxylysine groups.
That means it only deposits when you are low in vitamin C.
Lp(a) is also extremely similar to plasminogen.
The plasminogen receptor is responsible for converting plasminogen into plasmin, an active enzyme that breaks down fibrosis.
Because Lp(a) antagonizes the plasminogen receptor, it can lead to plaque buildup.
“No significant difference was found between the two groups with respect to blood pressure or serum triglyceride levels. Thus, serum Lp(a) levels correlate better with graft stenosis than serum cholesterol or triglyceride levels.”
By all accounts, Lp(a) is expressed under vitamin C deficiency as a protective measure.
What it does is strengthen the vascular walls by sparing fibrin.
This keeps us from bleeding out when we have a low collagen production rate and allows us to live longer when vitamin C isn’t available.
Atherosclerosis occurs only in the arteries, not in the veins – a fact that makes little sense when viewed under any other paradigm.
Nothing accounts better for the scientific data than this one intuitive mechanism.
And the correlations to lipoprotein(a) are so strong that cardiovascular disease cannot even be understood without it:
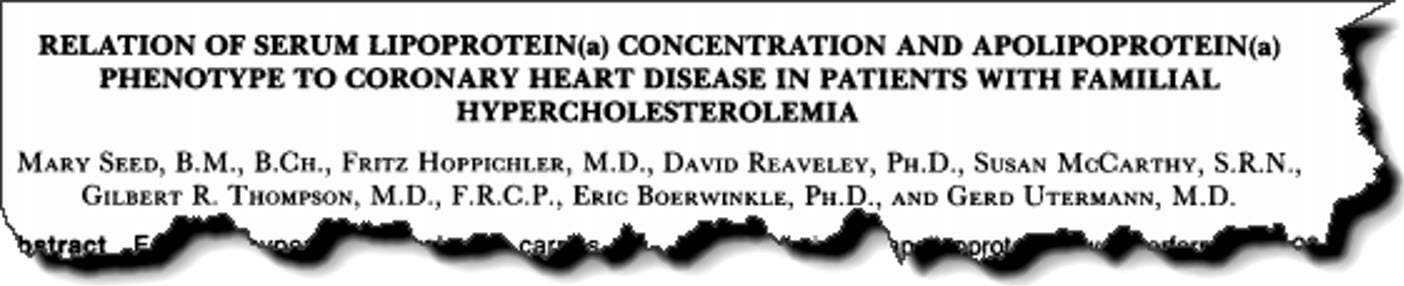
This study compared two groups of patients with familial hypercholesterolemia.
54 of these subjects had cardiovascular disease and 61 did not.
The researchers drew blood from the subjects. Then they centrifuged the blood and identified the cholesterol in each lipoprotein fraction.
They also collected data from the participants about their sex, age, and smoking habits.
“The median value of lipoprotein(a) was again found to be much higher in the patients with CHD than in those without CHD (57 vs 22 mg per deciliter).”
They found that lipoprotein(a) was the most significant predictor of cardiovascular disease…
They also found that cholesterol has very little to do with it.
You could even go so far as to say that cholesterol had absolutely nothing to do with it.
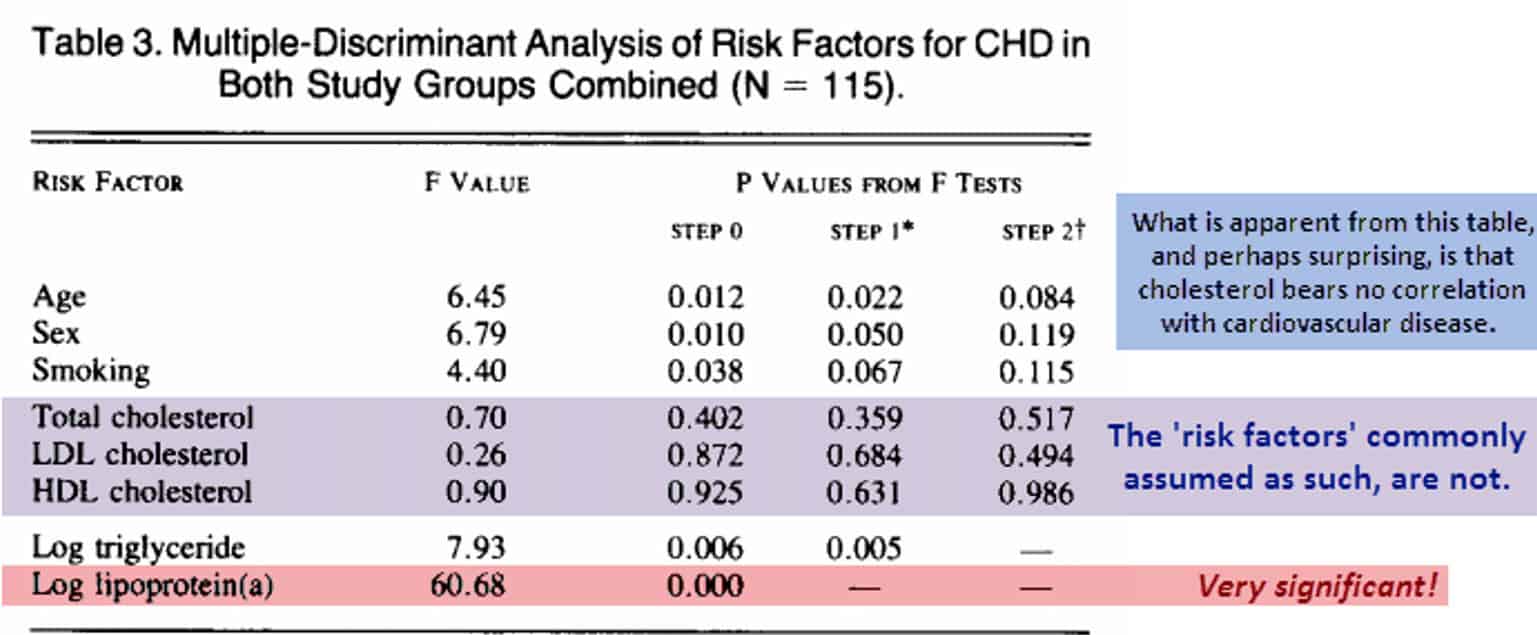
So-called “bad cholesterol” had nothing to do with it. And “good cholesterol” had nothing to do with it either.
Foregoing the absurdity of attributing silly names to cholesterol, the startling fact is that cholesterol isn’t much of a risk factor.
In the study, even smoking turned out to be relatively insignificant.
And this is easy to explain: Smoking cigarettes lowers plasma vitamin C levels, probably by reacting with nitric oxide.
Smokers simply need to take more vitamin C and gamma-tocopherol. Or get those things in food.
They could even buy ammonia-free tobacco, which would probably form much less nitric oxide upon combustion.
“No significant differences were observed between the two groups in serum total cholesterol, HDL cholesterol, or LDL cholesterol.”
And this study showed that simply being male is a risk factor for cardiovascular disease…
But this could be logically explained by two factors:
- On average, men retain more iron (for obvious reasons), and iron is notorious for oxidizing vitamin C.
- Men usually have higher blood pressure due to stress, thanks to adrenal output and catecholamines (hormones).
Although the study showed that cholesterol is unrelated to cardiovascular disease, regardless of whether it is “bad” or “good” cholesterol, triglycerides were implicated.
But they did not do a fatty acid analysis on the triglycerides to determine how many were saturated, mono-unsaturated, omega–6 unsaturated, and omega–3 unsaturated.
The potent platelet aggregation factor thromboxane A2 can only be made from arachidonic acid. And that is a toxic omega–6 fatty acid.
Consistently we see that this omega−6 fatty acid and its precursor, linoleic acid, are substantial risk factors for ischemic heart attack, stroke, clotting disorders, and bleeding time.
Salicylates inhibit stroke by preventing the formation of thromboxane A2, which is a prostaglandin product that originates from cyclooxygenase.
Tokelau islanders consume 60% of their energy as saturated fats, derived mostly from coconuts and animals they feed with coconuts. Cardiovascular disease is rare in this population, and so are their triglyceride levels of 150 mg/dL (Stanhope, 1980).
So even if short-chained saturated triglycerides could be considered a risk factor for cardiovascular disease (which I sincerely doubt), eating them does little towards raising serum levels anyway.
Our bodies metabolize these fatty acids so quickly that hyperlipidemia is better explained by hypothyroidism, diabetes, and even excessive retinol (vit A1) supplementation.
“We conclude that the occurrence of CHD (coronary heart disease) among patients heterozygous for familial hypercholesterolemia is influenced by lipoprotein(a) levels…and that this effect is independent of other risk factors.”
If this were the only study, you might suppose it is a peculiar outlier.
Especially when you weigh it against the backdrop of propaganda that saturated fat and cholesterol cause cardiovascular disease.
Yet most studies are actually 100% in accord with this one… far too many to contain within one article.
But there is constantly more proof that both lipoprotein(a) and thromboxane A2, if combined, account for nearly all cases of cardiovascular disease.
Knowing this makes prevention easy.
And it lowers the chance that a snake oil salesman will be able to convince you otherwise:
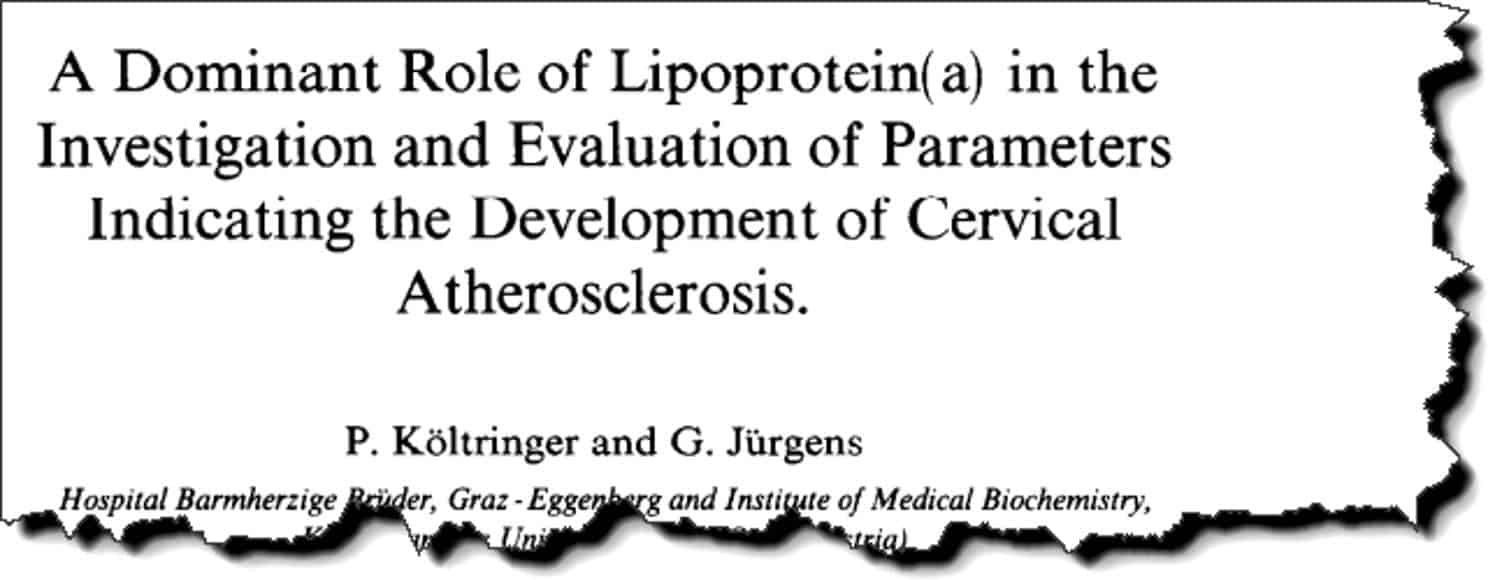
This study had roughly the same number of subjects as the other, including 52 survivors of stroke and 48 normal controls.
All subjects were over the age of 40.
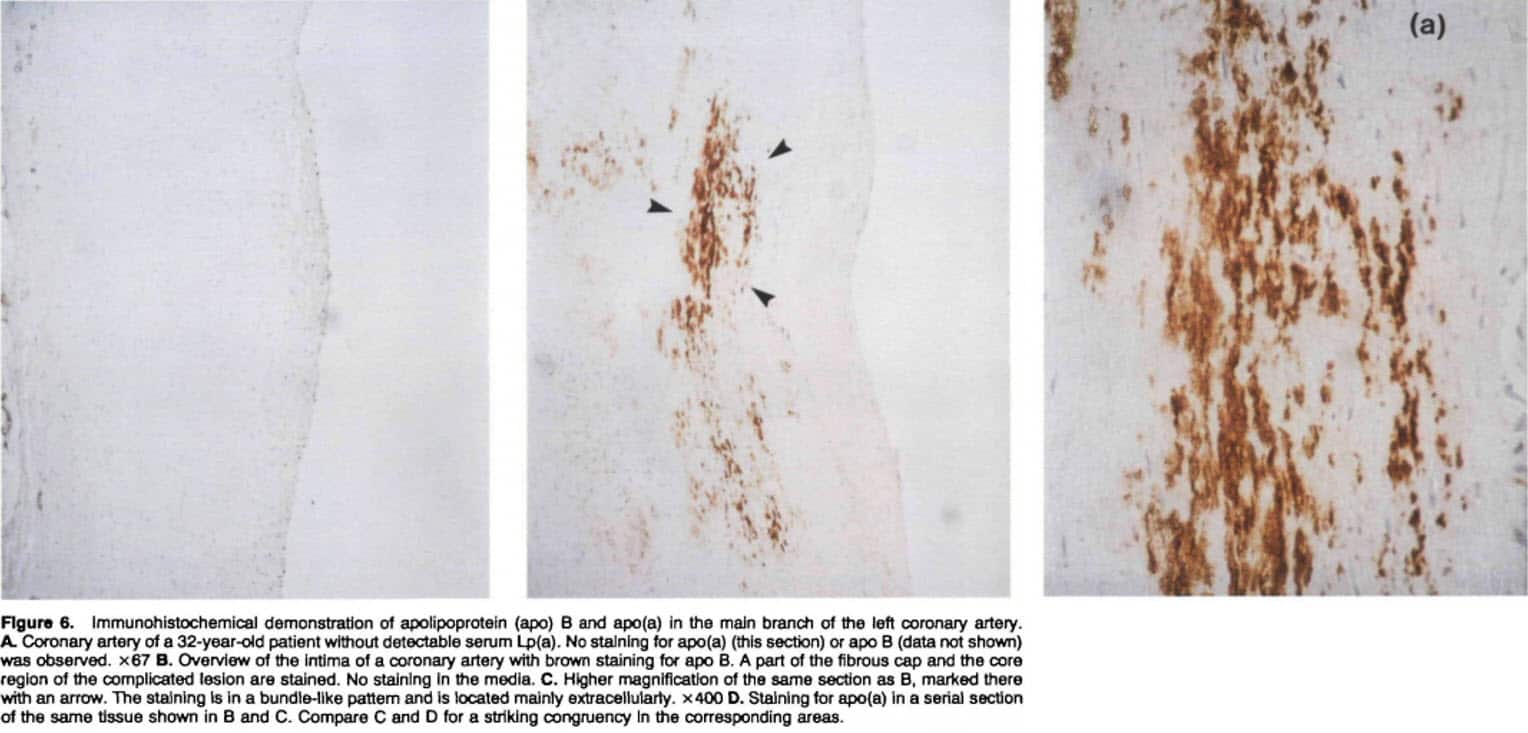
The researchers examined the carotid artery of the subjects, ostensibly because the blood clots that had previously induced their strokes originated there.
“Of all parameters investigated, Lp(a) showed the strongest association with formation and progression of atherosclerotic plaques in CA.”
Besides the usual blood parameters, the researchers also took into account hypertension, diabetes, and smoking.
Again, it turned out that Lp(a) was the single greatest risk factor.
Smoking, again, turned out to be entirely unrelated, so they didn’t include it in the graph (below).
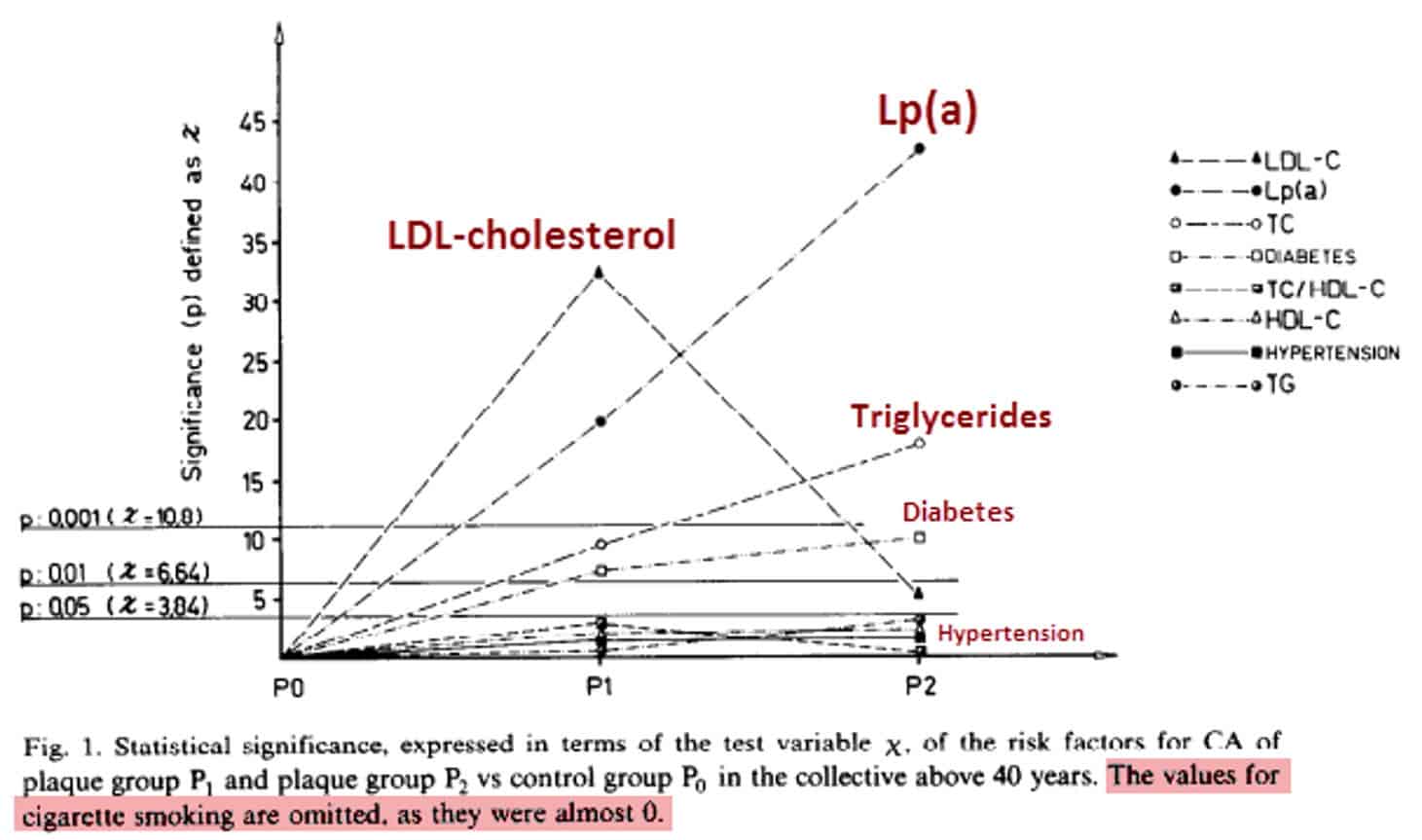
Besides LDL cholesterol, all of the assumed risk factors gain significance when you read from left to right – or through the three groups representing:
- (P0) the control group
- (P1) the medium-plaque group
- (P2) the high-plaque group
But, most Lp(a) is actually found in the low-density lipoprotein fraction.
In all of these studies (and the others I’ve seen), all of the small 10–20% increases in LDL cholesterol in CHD groups can be accounted for by the cholesterol contained within lipoprotein(a).
“The correlation between Lp(a) and LDL cholesterol levels found in the present study was hardly unexpected, since the common clinical method for estimating levels of LDL cholesterol actually measures Lp(a) cholesterol as well.”
The studies that actually separated the lipoprotein(a) from the LDL fraction found that the risk from LDL cholesterol evaporates.
LDL cholesterol risk is simply a low-fidelity way of measuring Lp(a) cholesterol, while the LDL particle itself – when defined as the distinct protein and not the “blood fraction” – demonstrates essentially no risk whatsoever.
And we can say the same about total cholesterol. You can see that in this study’s data tables:
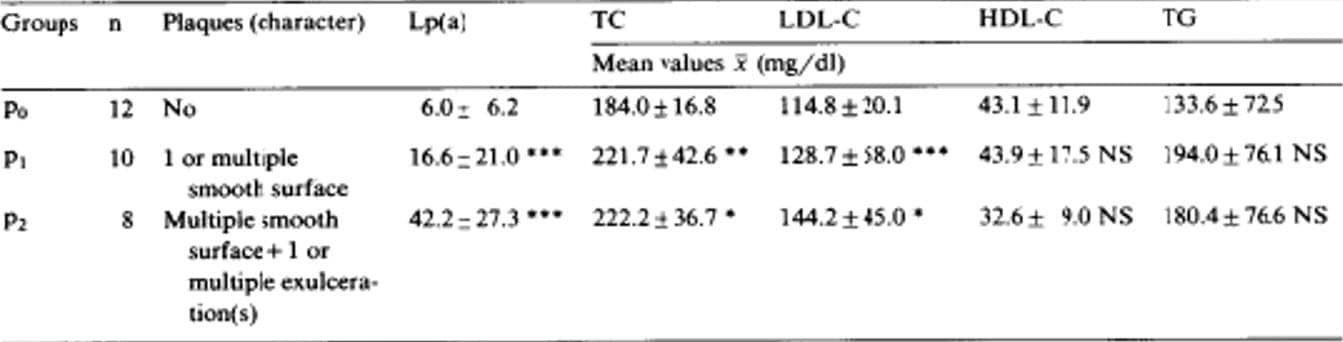
The presence of the additional Lp(a) observed in cardiovascular disease explains the increase in total cholesterol – and also the specific increase in the LDL fraction.
Total cholesterol, LDL cholesterol, and HDL cholesterol have very little relevance as compared to lipoprotein(a).
“However, we have no explanation for the rather weak significance of LDL cholesterol in both groups with arterial plaques.”
Hypertension and smoking were also mildly correlated in this study.
It seems likely that we could control higher blood pressure taking extra vitamin C, which would strengthen the arteries by increasing collagen turnover.
And the same is basically true of smoking, which can only be correlated to the extent it lowers vitamin C.
The small but notable correlation with diabetes is probably best explained by omega–6 fatty acids, common to both conditions.
But regardless of the other factors, it’s undeniable that Lp(a) obscures all others in importance.
While it’s true that genetics can influence the concentration of circulating Lp(a), the liver still requires a vitamin C deficiency for this to be expressed, apparently.
We all have DNA that encodes Lp(a). But that is only going to become a problem if your diet contains too many cooked foods and you don’t take vitamin C supplements.
Vitamin C is one of the most – if not the most – heat-labile vitamins (along with thiamine, niacin, and folate).
This is all consistent and I’ve seen no exception to these trends.
Okay, now I am probably flogging a dead horse (though it is a horse that should be flogged).
But, to demonstrate the reliability of these trends, here is one more article:
This study determined the atherosclerosis content of arterial bypass veins (the veins they take from your leg and implant near your heart).
You’re going to see the word “stenosis” in this study. Stenosis comes from the Greek word for “narrow.”
We use it in reference to the constricted regions of arteries, intestines, spinal canals… things like that.
This study had 135 subjects in the stenosis group and 32 subjects in the no-stenosis (or control) group.
The control patients had previously received a bypass, so their blood parameters are on the high side.
And, as in the other studies, the single factor most correlated with atherosclerosis was Lp(a).
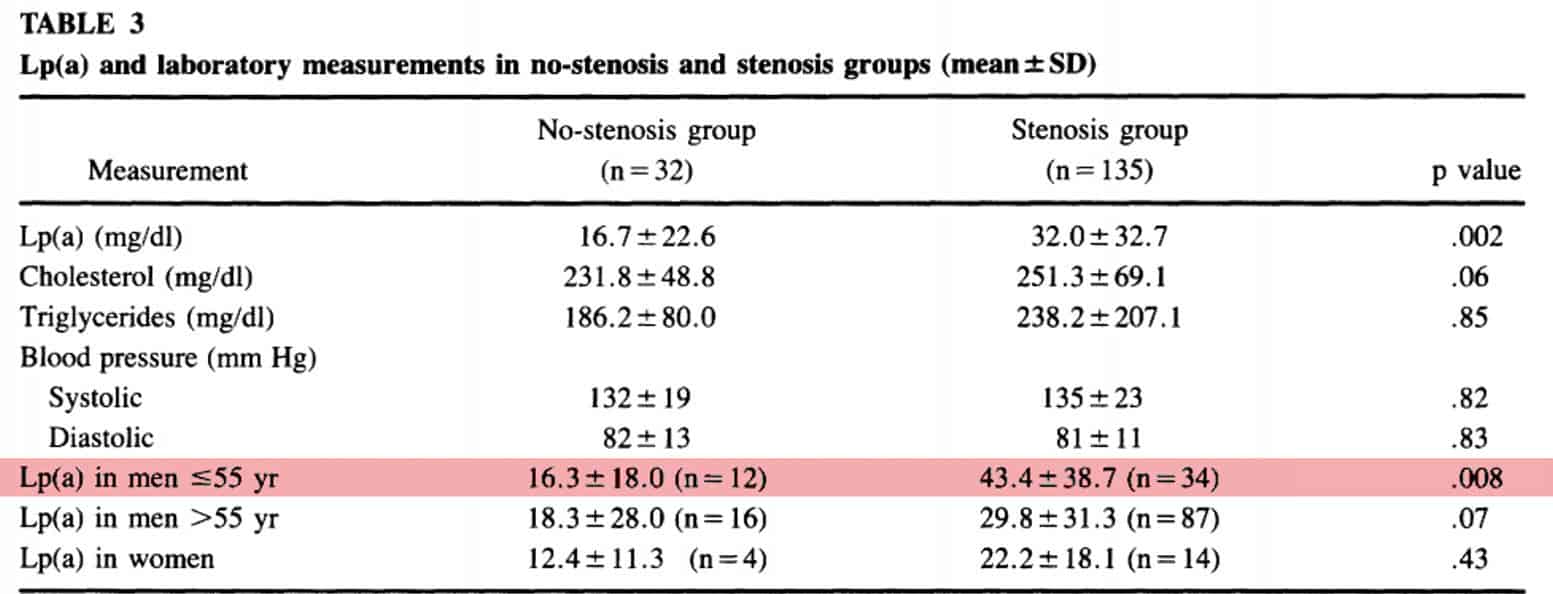
The difference would be even more extreme if random controls had been used – people with no previous history of cardiovascular disease.
It’s not uncommon to see Lp(a) in the single digits when expressed in milligrams per deciliter. The control group in the previous study had an average value of 4.0 mg⁄dL.
Just as in that study, the 8.4% increase of total serum cholesterol can easily be explained by the presence of that contained inside lipoprotein(a) – an additional particle not always present that hasn’t been correlated with much of anything besides DNA polymorphisms and the ability of a species to synthesize vitamin C.
“Although the total serum cholesterol levels in the stenosis group were slightly higher than in the no-stenosis group, that difference was only of borderline significance. No significant difference was found between the two groups with respect to blood pressure or serum triglyceride levels.”
So this is all pretty obvious. And it has been since the 1990s.
But the medical industry has relegated lipoprotein(a) to an ancillary role since then.
The AMA emphasizes much more speculative risk factors such as total cholesterol, saturated fatty acids, smoking, diabetes, and hypertriglyceridemia.
The AMA’s propaganda does not emphasize LP(a) as a factor.
This seems almost unbelievable the first time most people hear about it.
Maybe that’s because the mass media always gives the impression that vitamin C is merely something you give to kids when they have a cold.
When we extrapolate this superficial view onto a serious disease – and one that only adults get – we just assume on a subconscious level that using vitamin C would be ineffectual.
We may even find the idea comical.
Yet ascorbic acid doesn’t change its function when: (1) we call it something else, (2) we set its RDA at only 60 mg⁄d, or (3) we put it inside fruit-shaped chewables and market them to children.
Ascorbic acid is indispensable for synthesizing collagen, the strongest structural protein in the body.
“Graft stenosis was not associated with previous myocardial infarction, hypertension, obesity, diabetes, or smoking…A stepwise increase in mean Lp(a) was found in groups of patients with increasing vein graft stenosis. At a serum Lp(a) level of 31.6 mg/dl or above, 92% of the patients demonstrated vein graft stenosis.” –Hoff
“Lp(a) levels were found to correlate with those of LDL cholesterol. Since Lp(a) is precipitated by heparin-manganese during the procedure for measurement of HDL cholesterol, the value calculated for LDL cholesterol actually represents cholesterol contained in both LDL and Lp(a).” –Dahlen
“Among men 55 years old or less in our study, Lp(a) levels above 30 mg/dl were associated with an average 58% increase in coronary lesion score.” –Dahlen
“In the random populations, no direct relation was found between serum cholesterol or triglycerides and Lp(a) lipoprotein levels.” –Walton
“A unique cholesterol-rich lipoprotein, lipoprotein Lp(a), has been identified which not only can be confused with low-density lipoproteins, but has also been associated with premature cardiovascular disease.” –Gurakar
——Important Message—–
How to have perfect blood sugar
- You will not have to learn to give yourself shots.
- You won’t have to test your glucose levels constantly several times during the day, every day.
- AND you won’t be diabetic anymore.
What’s changed?

ASA is a very old medicine… But recently, scientists have found out that it reverses Type 2 diabetes.
ASA, it turns out, kick-starts your body into burning sugar again.
So you will always have normal blood sugar thanks to ASA.
You’ll go to the lab, and they’ll say “your blood sugar is normal.”
Click here to discover how to use ASA and reverse your diabetes
————–


Leave a Reply