
This makes men bigger and thicker down there without any device, pill, or weird jelqing technique…
—-Important Message From Our Sponsor—-
1038 men are using this secret method for a bigger wang

The reason it works is known as “cytomechanical elongation.”
It was developed by a nerdy surgical device engineer who wanted to add permanent length to his member…
Because all those other ways only boost your size temporarily…
But this breakthrough method gets men growing again down there naturally, even if he finished growing decades ago.
It’s like hitting puberty at age 50 and beyond. And only 1038 men are using it so far.
But now the geeky engineer is letting some additional men use the method — a simple way to turn on cytomechanical elongation in ANY man’s body…
———-
Surprising reason coconut oil seems to promote long life
Candida albicans is a ubiquitous microorganism present on everyone’s skin and in everyone’s intestines.
So due to its prevalence, the term “Candida infection” can be seen as somewhat of a misnomer; more appropriate could be “Candida proliferation,” or “Candida in invasive form.”
Because Candida is actually impossible to avoid.
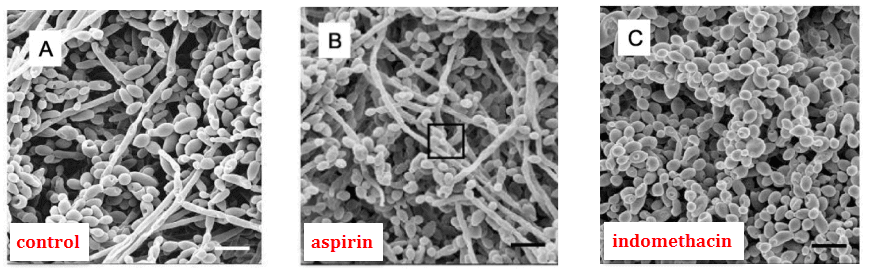
And it’s dimorphic: Candida albicans exists as both in yeast and fungal form — creating invasive hyphae upon stimulation:
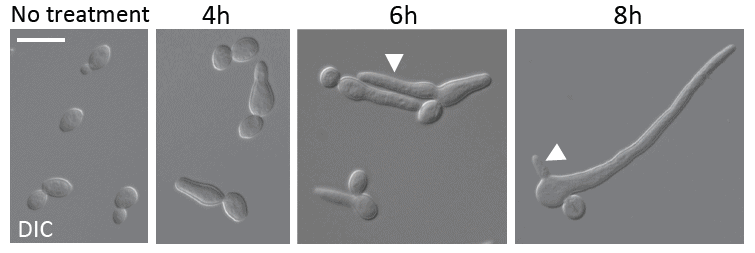
Only the fungal, or mycelial form is considered pathological.
The hyphae which bud out of Candida albicans allows it to invade tissues, which can actually be life threatening in immunosuppressed people.
The question which then arises is…
Why does it only proliferate in some people when everyone has it normally on their skin?
The answer turns out to be quite simple…
Candida albicans responds to certain morphogenic stimuli.
Certain small molecules in its local environment which can either suppress it or cause it to bud‐out hyphal projections, multiply, form so‐called “biofilms,” and invade tissues.
These morphogenic stimuli — or growth factors — are known and they are derived from food
Knowing how Candida albicans grows in response to just two signals sheds light on the question of why some people have Candida “infections” some of the time, while other people have Candida infections all of the time — or not at all.
This study was done as a logical continuation of other studies which had noted certain trends on Candida growth:
It had been long‐known that serum from some individuals could stimulate Candida growth, and in 1964 the Candida factor was found associated with albumin — the blood protein.
Albumin itself was actually thought to be the growth factor by some, but after pure albumin was shown ineffective that idea had to be discarded.
Whatever this was exactly, this Candida‐stimulating factor had been later shown to pass through a 1‧kDa membrane — a hole to small for albumin to pass through.
In 1990, prostaglandin E₂ was shown to transform Candida into the hyphal form. Prostaglandin E₂ normally binds to albumin.
And PGE₂ is formed from two dietary fatty acids only, linoleic and gamma-linolenic acid.
These are the only fatty acids which can form arachidonic acid, the only precursor to prostaglandins.
The 3-series prostaglandins can be made in our bodies from either stearic or oleic acids. These are much weaker than the 2-series and represent our natural, safer lipid hormones.
The 2-series prostaglandins create interference in our bodies. We had only started eating linoleic acid later in evolution, after migrating away from the tropics to eat grains and seeds.
So since one prostaglandin had been shown to stimulate Candida, these researchers had decided to test them all:
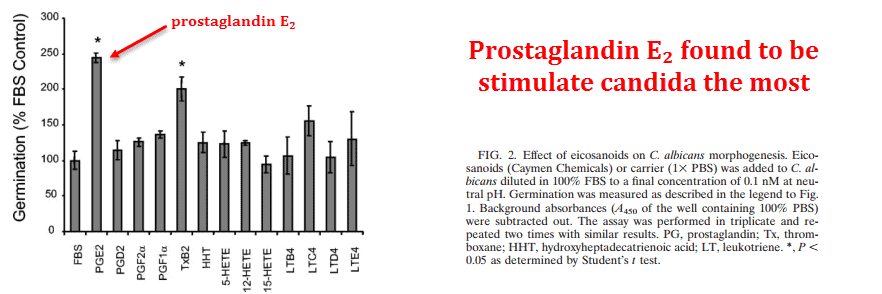
And others were found less‐effective than prostaglandin E₂.
The second most‐effective was thromboxane B₂, which is also made from arachidonic acid — the same precursor which creates prostaglandin E₂.
Arachidonic acid in turn only be formed through ingestion of the long‐chain omega-6 fatty acids.
So these dietary PUFAs would then seem almost necessary for Candida transformation.
They had even tested a wide array of other lipids, both unsaturated and saturated, and most fatty acids did nothing:
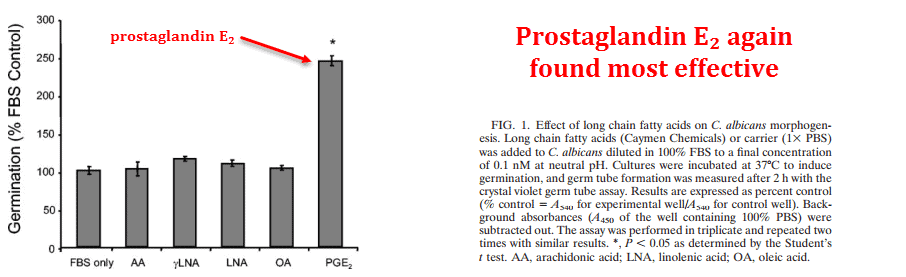
Except for one other one: butyric acid, which had inhibited it.
Butyric acid is formed by lactic acid bacteria, or so‐called “good bacteria.”
They showed that this is how it really inhibits Candida — not by simply “crowding it out” or displacing the yeast.
This is a short chain fatty acid, and could be why coconut oil and yogurt seem to work.
The short chain fatty acids capric, caproic, and caprylic are very close in size and they can be further reduced by intestinal bacteria to this slightly shorter butyric acid.
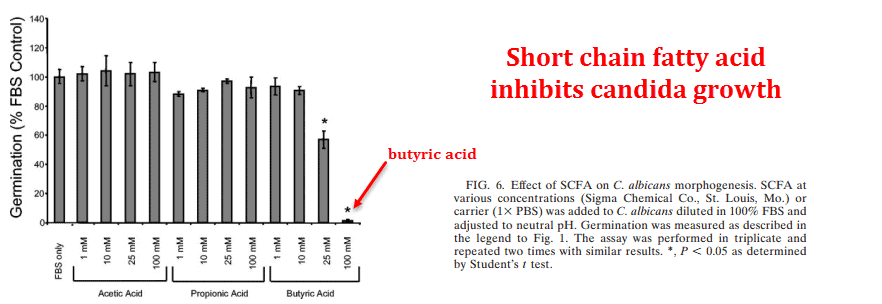
Antibiotics kill this so‐called “good bacteria,” lowering butyric acid in the intestines which can lead to Candida proliferation.
So why prostaglandin E₂ and no other? The same researchers showed a few years earlier that Candida actually produces prostaglandin E₂ as a hormone, and actually needs it to grow:
They had discovered that prostaglandins were naturally being formed by Candida albicans at a total concentration of 1,800‧ng/L.
They used two techniques to measure this — both ELISA and chromatography — so it’s conclusive.
And Candida could do this using only glucose and amino acids. It didn’t even need an external source of fatty acids.
So Candida albicans normally exists everywhere — synthesizing small amounts of prostaglandins for signalling yet will multiply using external sources.
They showed, as a formality, that Candida‐derived prostaglandins could do everything that synthetic prostaglandin E₂ could do — including downregulating TNF-α and increasing IL-10.
This shifts the immune system in a way that makes it less effective.
Candida tricks the host cell with prostaglandins.
‘Fungal PGE₂ and synthetic PGE₂ enhanced the yeast-to-hypha transition in C. albicans’ ―Noverr
And once it has turned hyphal and invaded the host, it can become even more invasive by using our own prostaglandins.
So avoiding omega-6 fatty acids is good for yet another reason besides for avoiding cancer, hair loss, and arthritis.
It seems as if many, if not most, modern health conditions can be explained simply by a few dietary factors — and by linoleic and gamma‐linolenic acids specifically.
Humans aren’t birds, rodents, or horses, and we certainly hadn’t been eating grains and seeds while living in the tropics before we’d even learned how to make fire.
‘Thus, these signal molecules (prostaglandins and other eicosanoids) appear to be generated via a conserved biochemical pathway that is important in both fungal metabolism and host defense.’ ―Noverr
It has been estimated that during paleolithic times, humans were eating ω−6/ω−3 at a ratio of around 1∶1. Today, we are eating ratios around 17∶1. (Simopoulos, 2002).
This simple fact can logically explain most disease, high methionine perhaps the rest of it.
These fatty acids can be found in grains, seeds, nuts, and eggs.
‘The data shown in Fig. 2 suggest not only that a cyclooxygenase-dependent metabolic pathway is found in C. albicans and C. neoformans but that blocking this pathway kills the yeast.’ ―Noverr
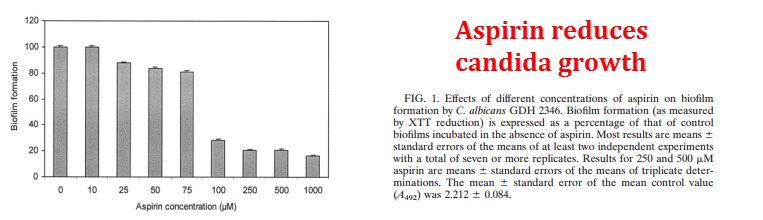
But since it’s difficult to eliminate all linoleic acid from the diet, certain other things — like aspirin — can help.
Knowing that Candida albicans needs prostaglandins to survive, biochemists from England decide to test COX‐2 inhibitors on it.
Cyclooxygenase‐2 (COX‐2) is the enzyme required to form all prostaglandins from arachidonic acid.
They had found quite predictably that they could — all of them.
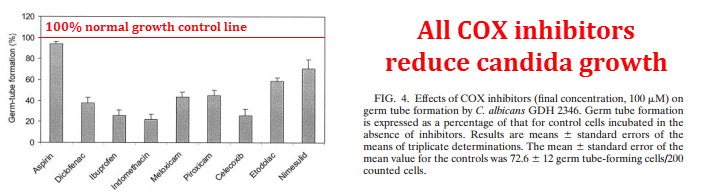
This basically adds more proof that prostaglandins are Candida hormones and absolutely essential for fungal growth.
Although aspirin was the least powerful one, gram‐for‐gram, its low toxicity means you can take much more than the others.
‘The inhibitory effect on biofilms appeared to be dose related. Over 70% inhibition was observed at aspirin concentrations between 100 μM and 1 mM. […] Aspirin concentrations of 50 to 200 μM can be achieved in humans by the use of therapeutic doses…’ ―Alem
These effects were nullified by prostaglandin E₂, showing yet again — in a different way — that prostaglandin E₂ is essential.
Although cancer, hair loss, and arthritis seem somewhat multifactorial and have a few causes, Candida “infection” appears to have one only cause: prostaglandin E₂.
And there’s even epidemiological evidence showing this to be the case — done with females (Witkin, 1988):
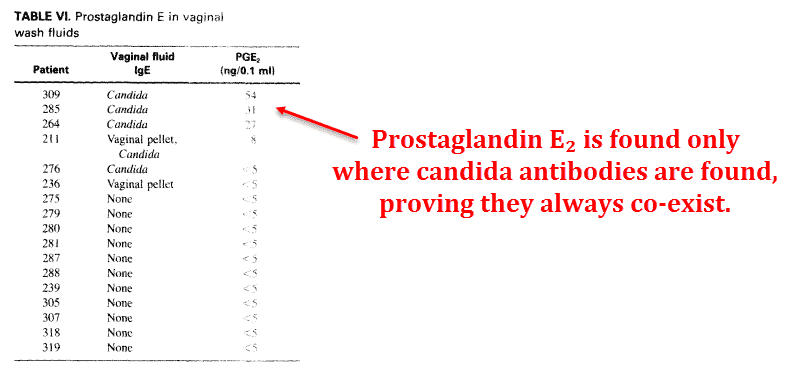
So there can be little doubt now as to why some people have athlete’s foot and sinus infections, while others do not.
I think most people know that food is related to Candida in some way, but not exactly sure how.
But it seems quite simple: Candida albicans turns pathological on contact with the host’s prostaglandins, a process which can be inhibited by short‐chain fatty acids in the diet or from those produced by ‘good bacteria’ in the intestine.
And if allowed to get out of hand, they can modify the immune system by creating prostaglandins of their own — further exacerbating and facilitating the issue.
‘Given the biological activity of the purified fungal eicosanoids, they have the potential to mediate host-pathogen “cross talk,” in which the pathogen can down-regulate (local) host immune responses at the site of infection and the host can inadvertently augment pathogen virulence. The result of such interactions could be an immunological stalemate, i.e., chronic low-grade infection or parasitism. The most common feature of fungal infections is their chronic persistence within tissues of otherwise healthy individuals, ranging in severity from athlete’s foot to chronic vaginitis to pulmonary granulomas.’ ―Noverr
—-Important Message About Killing Bad Bacteria—-
This cleans bad bacteria out of your organs — try it for free
My new protocol cleans men’s organs out, even their male organ.
And the result is much better health and rockiness.
For a limited time, I’m letting men try it for free.
Clean Organ Protocol just for men — click to try
———-

Noverr, Mairi C. "Regulation of Candida albicans morphogenesis by fatty acid metabolites." Infection and immunity (2004) http://iai.asm.org/content/72/11/6206.short
Noverr, Mairi C. "Pathogenic yeasts Cryptococcus neoformans and Candida albicans produce immunomodulatory prostaglandins." Infection and immunity (2001) http://iai.asm.org/content/69/5/2957.short
Alem, M. "Effects of aspirin and other nonsteroidal anti- inflammatory drugs on biofilms and planktonic cells of Candida albicans." Antimicrobial agents and chemotherapy (2004) http://aac.asm.org/content/48/1/41.short
