
Limit these foods if you want to avoid diabetes
—-Important Message—-
This will guarantee you’re the best lover she’s ever had

There are really only two ways to give her a nice, long, satisfying stretch of penetration that ends in a pleasure explosion for her…
1. You can learn to last a really long time during intercourse, without blowing your load… (and without having to rely on costly pills, creams, etc.)
OR…
———-
These 5 foods can lead to insulin resistance in men
Most people are fully aware that diabetics have high blood glucose and are “insulin resistant,” but very few of them know why.
In fact, even the majority of medical doctors are clueless.
Despite all the requisite evidence having been published, most physicians would care less about reading them as they’re paid to hand out chemical treatments.
Most cases of insulin resistance, as it turns out, are actually caused by just a handful of dietary factors…
An excess of ω-6 fatty acids can induce it, as well as a deficiency in thiamine, chromium, magnesium, manganese, and/or chiro‑inositol.
Hundreds of epidemiological, experimental, and clinical studies have together shown that these are the five main nutritional risk factors.
These three mineral ions (Cr3+, Mg2+, Mn2+), thiamine, and chiro‑inositol are all required for the insulin signalling pathway.
Since all of these are necessary for transmitting insulin’s signal after it binds with its receptor, a deficiency in any one can be perceived as “insulin resistance.”
In other words, a deficiency of just any one of these dietary factors will prevent insulin from working efficiently.
Magnesium is a cofactor for multiple enzymes involved in glucose metabolism, too many to list, while Cr3+ is the cofactor of tyrosine kinase — one of the two enzymes activated by the insulin receptor.
The other enzyme activated through the insulin receptor is GPI‑phospholipase C which, upon hormone ligand binding, releases a chiro‑inositol‑containing polysaccharide from cell membrane phospholipids.
This polysaccharide was historically called the “pH 2.0 insulin mediator” and was discovered even before the tyrosine kinase pathway had been known.
Now after being released from the cell membrane, the chiro‑inositol‑containing “insulin mediator” chelates Mn2+ and then diffuses into the cell.
Once inside, the Mn2+ complex stimulates two very important metabolic enzymes: pyruvate dehydrogenase and glycogen synthase.
Thiamine is a cofactor for pyruvate dehydrogenase, the main reason why it’s important for glucose handling.
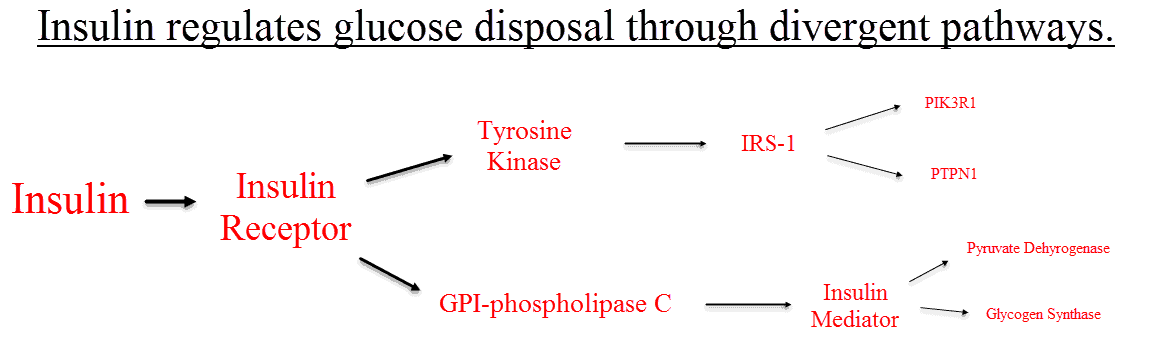
The complexity of these two divergent pathways, both being dependent on at least one cofactor, has led to a considerable amount of confusion over what causes diabetes type‑2.
There’s even been some confusion over what causes chiro‑inositol deficiency.
Some argue that it’s normally made within the body, while others are proclaiming an explicit dietary origin.
“ᴅ‑chiro‑inositol was neither synthesised endogenously from 2H-labelled water nor converted from [2H6]myo-inositol. ᴅ‑chiro‑inositol and pinitol in rodents appear to be derived solely from the diet.” ―Lin, 2009
There’s better evidence for chiro‑inositol having a dietary origin than an enzymatic one, but it matters little on a practical level because supplements are now available.
That is to say, chiro‑inositol supplementation works regardless of why it’s low to begin with.
Now to help choose between the dozens of supplements often claimed as being “antidiabetic,” below is some evidence in favor of chiro‑inositol being one of the more useful ones:
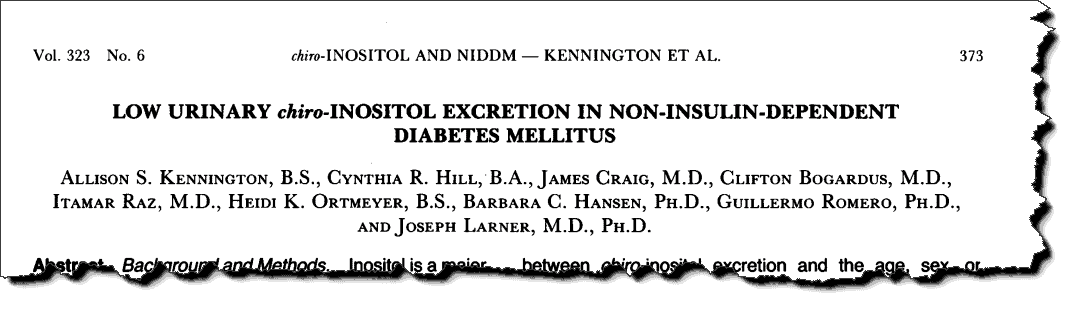
This study was a natural response to earlier ones showing that chiro‑inositol, a somewhat rare molecule in mammals, is an essential component of the “insulin mediator.”
And knowing just how important the “insulin mediator” was to proper glucose handling, these investigators had conducted the first trial on chiro‑inositol status in humans.
They recruited 26 normal subjects and 31 diabetics, as well as 11 individually‑caged monkeys all on the same diet.
They found that the average urinary chiro‑inositol excretion was 84.9 μmol⁄day in the normal subjects, yet only 1.8 μmol⁄day in the diabetics!
The normal subjects had excreted 47‑times more chiro‑inositol, a massive difference by any standard.
The same thing was noted between the two monkey groups and moreover, the trend carried over to tissue inositol concentrations.
On account of the researchers taking muscle biopsies from every subject during their hyperinsulinemic-euglycemic clamp studies…
They could now prove the excretion differences represented true deficiencies and not merely kidney resorption issues.
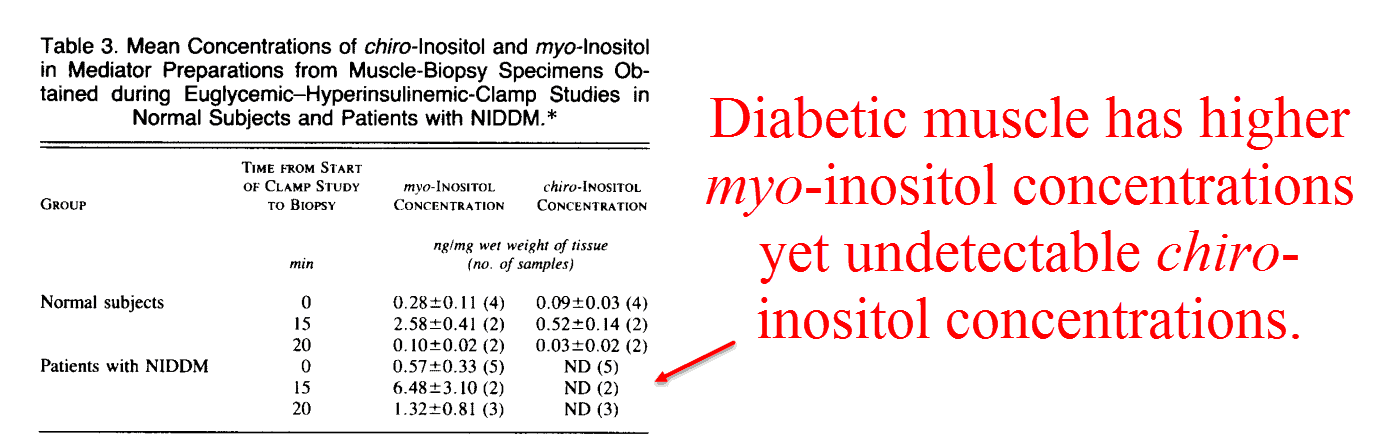
Just like the urinary excretion studies, the diabetics actually had higher myo‑inositol concentrations to offset their lower chiro‑inositol concentrations.
This high urinary myo‑inositol in diabetics is certainly nothing new and has been known for quite some time.
“The presence of increased amounts of [myo] inositol in the urine of patients with diabetes mellitus has been known for almost a century.” ―Daughaday, 1953
This is because unlike chiro‑inositol, myo‑inositol can be made in the body from glucose‑6‑phosphate.
The enzyme that accomplishes this is named myo‑inositol 1‑phosphate, and it has been well characterized.
On the other hand, no human enzyme capable of synthesizing chiro‑inositol from any source has ever been isolated.
Since the American Diabetic Association would likely prefer a genetic basis for diabetes, i.e. not a dietary one, this probably isn’t from any lack of trying.
If humans actually had an enzyme capable of making chiro‑inositol, it almost certainly would’ve been discovered by now.
And chiro‑inositol deficiency in diabetes isn’t an isolated finding either.
It’s been confirmed multiple times over, both in humans and in monkeys:
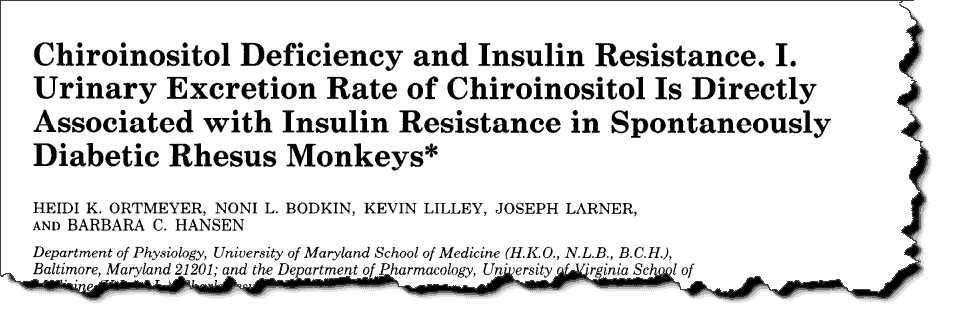
Continuing with the line of investigation he’d begun in the early ’70s, Joseph Larner provides some of the most compelling evidence for the chiro‑inositol regulation of insulin signalling.
Twenty‑seven monkeys of all ages were included in this study.
Each and every one was subjected to a glucose tolerance test, a blood sampling, a urine testing, a muscle biopsy, and an adipose tissue biopsy.
They found a good correlation between chiro‑inositol excretion and total insulin resistance (r = .65), and an even better one against it and the glycogen synthesis activity ratio (r = .73).
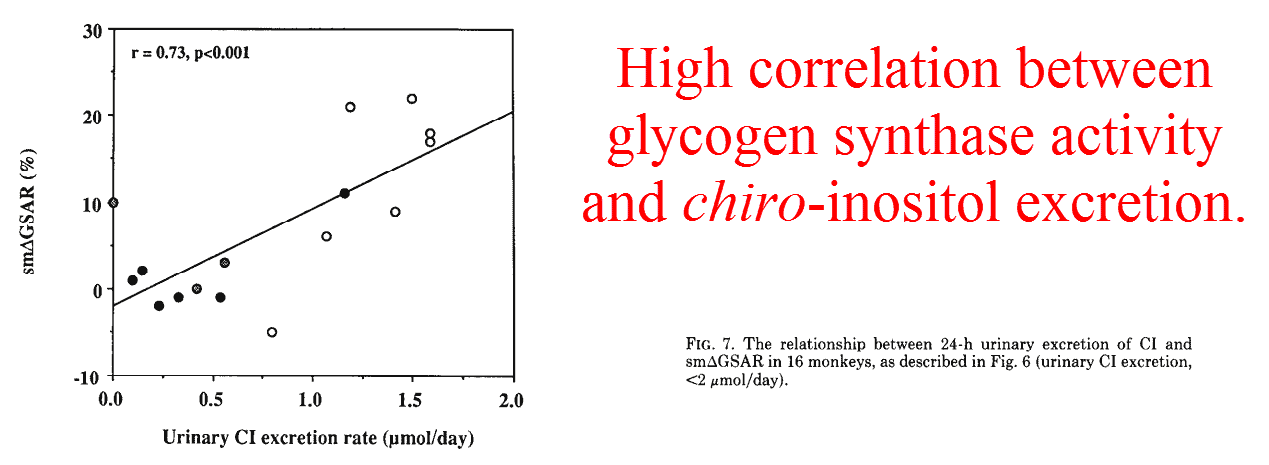
This is what you’d expect considering that glycogen synthase is one of the classic enzymes known to be regulated by “insulin mediator,” but what’s perhaps surprising is the strength of correlation.
This is even more impressive when considering the age range of the monkeys, which were between 6 to 23 years old.
If they would have adjusted for such things as thiamine, magnesium, chromium, and manganese it would probably be a perfect fit.
Later that same year they’d demonstrated something similar with pyruvate dehydrogenase phosphatase, the enzyme which activates pyruvate dehydrogenase via “insulin mediator.”
In that study they’d extracted “pH 2.0 insulin mediator” from both normal and diabetic tissues, thus demonstrating that its ability to activate pyruvate dehydrogenase phosphatase was impaired in the latter group.
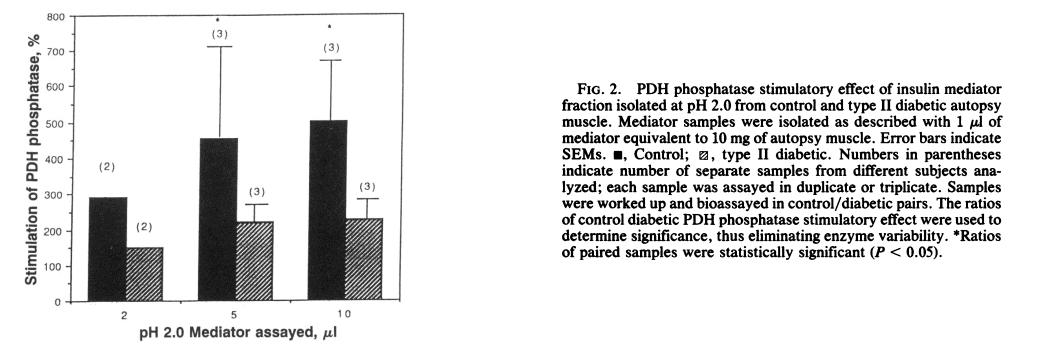
Since the “pH 2.0 insulin mediator” does not work without chiro‑inositol, this would imply that it’s replaced by myo‑inositol in the diabetics.
This is supported by the fact that there’s a weaker “insulin mediator” that elutes at pH 1.3 known to contain myo‑inositol, yet this only activates cAMP enzymes and has no activity on the more important ones.
This finding isn’t restricted to Americans either, as the same thing has been reported to occur in Asians:
This study had used 10 controls, 18 diabetics, and 8 people having impaired glucose tolerance.
Urinary chiro‑inositol was then determined, and all were given 75 grams of glucose + insulin to determine their “insulin sensitivity index.”
As with the data on monkeys, the results were astounding.
The correlation coefficient between insulin sensitivity (Si) and urinary chiro‑inositol was 0.766.
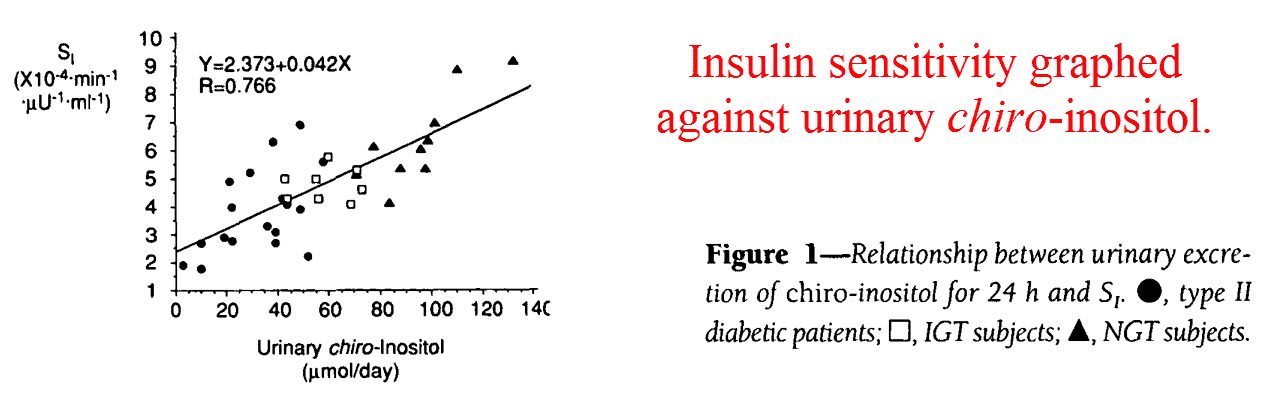
And again confirming the earlier studies, urinary chiro‑inositol concentrations had decreased in accord with diabetes status.
It was measured at 192 μmol⁄day in normal, 58.9 μmol⁄day in impaired glucose tolerance, and 32.2 μmol⁄day in diabetic subjects.
The expected counter‑trend was again observed with myo‑inositol, perhaps being the result of increased synthesis from high glucose‑6‑phosphate concentrations.
Yet this could also be an indication of diet. Little is known about the total inositol content of foods, much less about their stereochemistries.
“These data suggest a causal relationship between urinary chiro-inositol excretion and in vivo insulin resistance.” ―Suzuki, 1994
This trend was again confirmed six years later, this time in Germany.
The same inverse relation between chiro‑ and myo‑inositol was observed in diabetics, and also in their offspring.
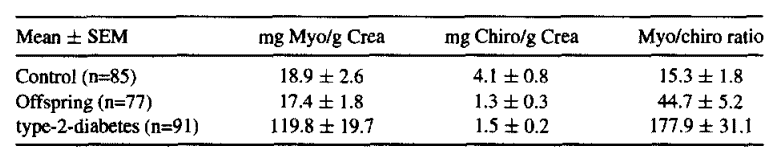
Studies such as these are often used to argue for a genetic basis of diabetes, yet everyone knows that children most often eat a diet similar to their parents’.
Yet as mentioned earlier, the exact reason for this inositol imbalance has little practical relevance because:
(1) supplements are available, (2) they have been shown to work regardless, and (3) little is known about the inositols in foods.
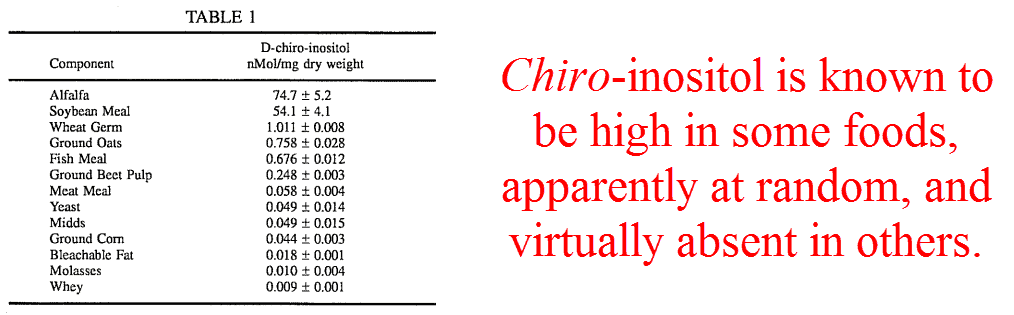
Chiro‑inositol has also been reported as being exceptionally high in citrus fruits, being most concentrated in mandarins.
This is especially good news because alfalfa doesn’t sound fun to eat and soy should be avoided at all costs.
The unusually high concentration of chiro‑inositol in citrus could also explain, along with naringenin, why the “grapefruit diet” had come to be seen as antidiabetic.
And chiro‑inositol isn’t just limited to insulin signalling, by the way.
Glycosyl‑phopshoinosotides have been shown to mediate the signalling of thyrotropin‑releasing hormone, thyroid‑stimulating hormone, interleukin‑1, and interleukin‑2.
This overlooked fact could explain, at least partially, both the immune dysfunction and hypothyroidism characteristic of diabetics.
This is also a good reason for everyone to be interested in chiro‑inositol, diabetic or not.
—-Important Message for Men With Prediabetes and Diabetes—-
This simple cellular smoothie is restoring erections in diabetic men
This smoothie increases cellular energetics that are very low in diabetic men.
The smoothie raises the NAD+ to NAD ratio.
This results in men becoming rocky down there — feeling blood rushing into their penile organ like it hasn’t in years.
And it reverses diabetes symptoms.
Here’s the cellular smoothie that can reverse diabetes in men, even type 2
———-

[1] Kennington, Allison. "Low urinary chiro-inositol excretion in non-insulin-dependent diabetes mellitus." New England Journal of Medicine (1990) https://www.nejm.org/doi/full/10.1056/NEJM199008093230603
[2] Ortmeyer, Heidi. "Chiroinositol deficiency and insulin resistance. I. Urinary excretion rate of chiroinositol is directly associated with insulin resistance in spontaneously diabetic rhesus monkeys." Endocrinology (1993) https://www.researchgate.net/profile/Heidi_Ortmeyer/publication/14772793_Chiroinositol_deficiency_and_insulin_resistance_I_Urinary_excretion_rate_of_chiroinositol_is_directly_associated_with_insulin_resistance_in_spontaneously_diabetic_rhesus_monkeys/links/5c13f9d14585157ac1c2e749/Chiroinositol-deficiency-and-insulin-resistance-I-Urinary-excretion-rate-of-chiroinositol-is-directly-associated-with-insulin-resistance-in-spontaneously-diabetic-rhesus-monkeys.pdf
[3] Asplin, Iain. "Chiro-inositol deficiency and insulin resistance: a comparison of the chiro-inositol and the myo-inositol-containing insulin mediators isolated from urine, hemodialysate, and muscle of control and type II diabetic subjects." Proceedings of the National Academy of Sciences (1993) https://www.pnas.org/content/pnas/90/13/5924.full.pdf
[4] Suzuki, Susumu. "Urinary chiro-inositol excretion is an index marker of insulin sensitivity in Japanese type II diabetes." Diabetes Care (1994) https://www.ncbi.nlm.nih.gov/pubmed/7882818
[5] Wahl, Hans Günther. "Non-diabetic first degree relatives of type-2-diabetes patients have a significant higher urinary myo-/chiro-inositol ratio compared to healthy controls and a significant lower ratio compared to type-2-diabetes patients." Diabetes Research and Clinical Practice (2000) https://www.diabetesresearchclinicalpractice.com/article/S0168-8227(00)81345-5/fulltext
