
This sleep position cuts off oxygen-rich blood flow

—-Important Message From Our Sponsor—-
Have you heard of the “Xersizer”?
It helps you give jaw-dropping performances to your wife, regardless of your age.
This Harvard trained doctor shocked the world with this discovery that helps men get the job done by improving penile blood flow.
There’s a bit of science involved…but this super easy trick turbo-charged my performance big time!
Here’s how to unleash better blood flow “down there” and perform at your best with her.
———-
Sleeping this way causes hypoxia — can cause “rockiness” problems
Sometimes people sleep with their heads covered up by blankets…
…often after waking up temporarily when lighting conditions interfere with their sleep.
Yet there are others who do this always and even in pitch darkness…perhaps as a comfort habit or to quickly increase under-blanket temperature.
And this has long been thought of as a more or less innocuous habit.
But a recent survey has shown a strong link between sleeping with head covered in blankets — and Alzheimer’s disease.
This survey was conducted by Barry Stanley, a statistical amateur and Canadian grade-school teacher with no credentials in epidemiology or biochemistry.
So some would tend to disregard the data for this reason – especially “turtle sleepers” who would prefer to think it is safe.
But his methods were actually not much different from some methods used in studies published in peer-reviewed journals.
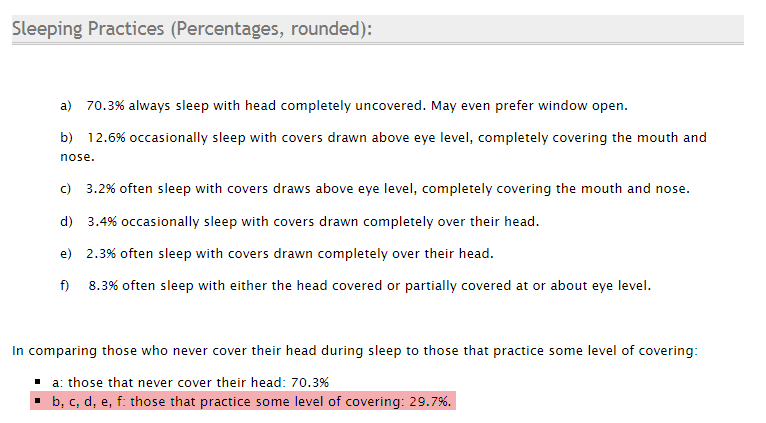
“92.8% of those who practiced any form of head covering while sleeping will suffer from either an early, middle, or late stage of dementia at or after 70 years of age.” (Stanley)
Such powerful correlations are hard to ignore, as his survey includes results from 443 people.
These findings are certainly statistically significant, despite the formal p-value not having been calculated by Stanley. (It’s not important that you know what a p-value is.)
Stanley proposes no real mechanism for the effect (of why covering your head with blankets causes dementia).
Now I’m going to talk about a condition called hypoxia – where the body or a region of the body is deprived of adequate oxygen supply at the tissue level.
Hypoxia as caused by other things – e.g. carbon monoxide poisoning or sleep apnea – has convincingly been shown to be correlated with both brain atrophy and reduced cognition.
And then there’s vascular dementia…a common form of dementia thought to be dependent on reduced cerebral blood flow. It is often caused by atherosclerosis.
Reduced blood flow can obviously limit the delivery of many important biomolecules, glucose among others.
But when it comes to sleeping with your head under the covers…
The contribution of reduced oxygen certainly cannot be discounted… It could be primary.
“Given the results as submitted, there is strong indication that head covering while sleeping has a significant impact on the occurrence and advance of dementia.” (Stanley)
Yet hypoxia and cerebral ischemia (inadequate blood supply) are nearly two sides of the same coin, as you will see…
Acute hypoxia induces rapid changes in the cells’ enzymes – meant to increase blood flow and thus acquire more oxygen.
Yet such changes ultimately diminish oxygen flow the moment normal air is breathed again.
This rebound effect could be caused by vasoconstriction (constriction of blood vessels).
Specifically, vasoconstriction induced by lowered concentrations of carbon dioxide (hypocapnic vasoconstriction).
Hypocapnic vasoconstriction is a well-established phenomenon. Since the 1940s, it’s been reliably shown to occur.
This may be expected to occur because carbonic anhydrase, the enzyme that turns carbon dioxide (CO2) into bicarbonate (HCO3−), is powerfully upregulated by hypoxia.
Lack of oxygen has also been shown to decrease dopamine in the brain…
Possibly this is because, in the formation of dopamine, we need oxygen added to tyrosine (an amino acid).
Although serotonin concentrations can also be found decreased after hypoxia, studies show that dopamine is more affected than serotonin.
Serotonin synthesis seems to depend more on tryptophan availability than oxygen concentrations.
“…it is thus suggested that the observed changes in tryptophan hydroxylation may in part depend on the changes in tryptophan availability. This did not seem to be the case concerning tyrosine hydroxylation and tyrosine availability.” (Hedner, 1977)
Yet such transient reductions are unlikely to persist for long.
And they cannot explain the reduced blood flow consistently shown in dementia.
Now, knowing what we know about hypoxia in general, you could reasonably expect “turtle sleeping” to temporarily lower cognitive function.
And since this practice tends to be habitual, you could perhaps rightly infer that people who sleep this way would have an increased risk of dementia.
And this practice isn’t any more common than dementia itself, with 11% of a 100-person sample in Massachusetts admitting to sleeping this way (King, 1972).
The ongoing survey by Barry Stanley (mentioned at the beginning of this article) includes more people than any other (443 people).
And it shows a nearly threefold higher prevalence in “undercover sleeping” (29.7%) among his participants.
He does, however, use a somewhat subjective graded scale including milder stages of dementia as response options:
This prevalence could be a bit artificial and subject to selection bias.
His survey can be freely taken online by anyone. So participants with this habit may be self-selecting more often via Google searches and word of mouth.
“100% of those who practiced the most serious levels of head covering (c, d, and e above) while sleeping will suffer from either an early, middle, or late stage of dementia at or after 70 years of age.” (Stanley)
Yet this is the only survey that correlates dementia strictly with undercover sleeping.
Although Stanley presents the data in a hard-to-grasp table format, it can be made more intuitive using graphing software.
The correlations are more convincing when restricted to the 70+ age group (especially when some sleeping grades are summed together).
But this graph shows the results of all 443 people with all grades separated as in the original table (graph made using desmos.com):
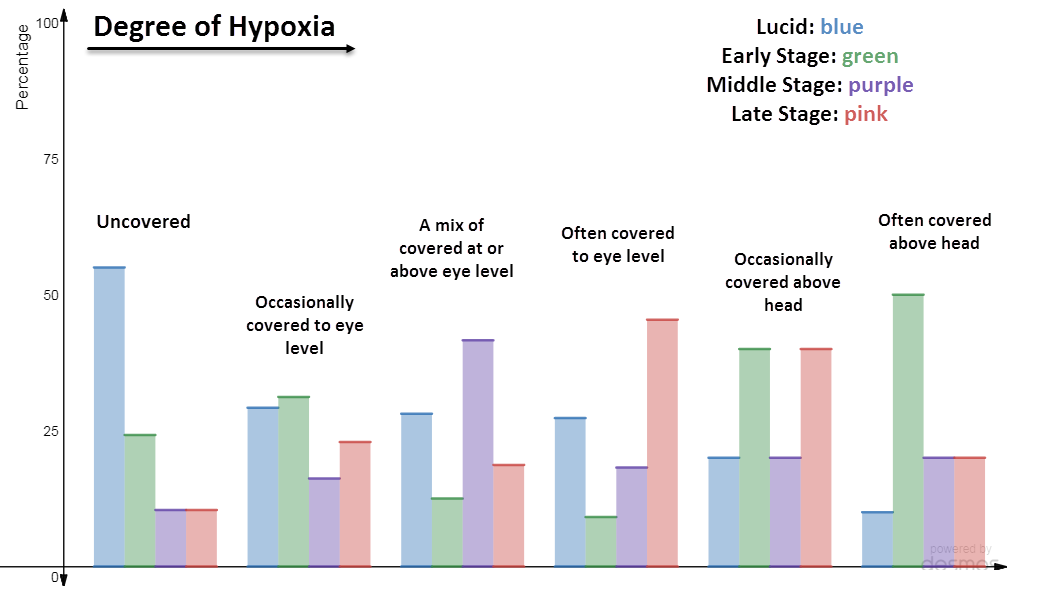
With additional degrees of blanket coverage – going from left to right on the graph – a general increase in dementia prevalence can be observed.
This data isn’t a perfect dose-dependent increase, of course, as the categories are somewhat subjective…
For instance: What is the difference in arterial oxygen between those who “often cover to eye level” and those who “occasionally cover above head”?
Since it also depends on such things as blanket weight, blanket porosity, and number of blankets used, you probably wouldn’t expect extremely convincing correlations anyway.
This is especially true when considering that dementia can be caused by other things as well, and not just strictly hypoxia.
Yet this trend is confirmed by a more elaborate study published in the Journal of the American Medical Association:
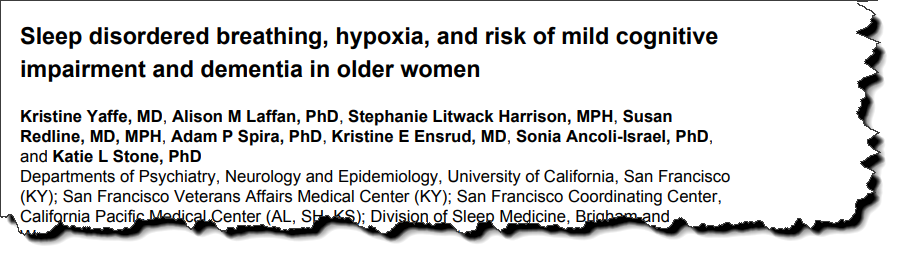
While this study was about sleep apnea and not about blanket coverage, the results are relevant because they determined arterial oxygen in 298 subjects during sleep.
And not only that, these researchers measured three separate indices of hypoxia:
- The oxygen desaturation index
- The time spent in oxygen saturation
- The total time spent in apnea
They recorded multiple parameters while the subjects were asleep, a process they termed “polysomnography.”
They also measured sleep fragmentation and correlated it to cognitive test scores five years later during the final analysis.
This was a prospective study, so it could determine specifically whether apnea had caused dementia and not vice versa.
After all was said and done, the only correlations between dementia and the polysomnography indices were those of hypoxia.
Sleep fragmentation had no bearing on the risk of dementia – only hypoxia did:
“Conversely, no significant association was seen for the sleep fragmentation or sleep duration measures of arousal index, wake after sleep onset, or total sleep time, before or after adjustment for covariates. Measures of hypoxia remained significant even after adjusting for covariates and baseline cognitive test scores…and sleep time in apnea/hypopnea…” (Yaffe, 2011)
These results are in accordance with carbon monoxide poisoning in humans and hypoxia studies in animals.
This study strengthens the supposition that hypoxia, whatever the precise cause, will lead to a cascade of events that lower brain function.
You might expect a few immediate effects from hypoxia such as lowered dopamine and decreased microtubule synthesis, reduced plasticity and remodeling rates, and a general reduced metabolism.
Yet carbonic anhydrase 9 is inducible by hypoxia. (As discussed above, carbonic anhydrases are a group of enzymes that turns carbon dioxide into bicarbonate.)
Carbonic anhydrase 9 lowers carbon dioxide, a powerful regulator of vasoconstriction and vasodilation:
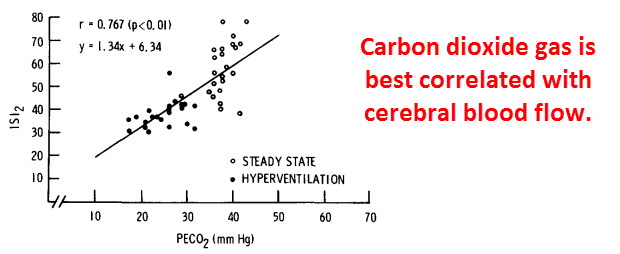
This hypoxic upregulation of carbonic anhydrase 9 has been shown to occur in many different cell types.
This effect is so reliable that carbonic anhydrase 9 is now considered a biomarker for hypoxia.
Scientists don’t often focus on the physiological function of this.
And when it is, they sometimes explain it by acidity (Svastová, 2004).
But it could be that carbonic anhydrase 9 is induced in a desperate attempt by the body to increase oxygen transport.
It’s well known that carbon monoxide exerts its toxicity by binding hemoglobin and reducing oxygen-binding…
Yet this property is also shared by carbon dioxide:
“In vertebrates, hemoglobin plays a central role both in the transport of oxygen from the respiratory surfaces to the tissues and in the transport of carbon dioxide in the opposite direction.” (Frank, 1991)
These two gasses compete with each other for binding to hemoglobin.
So reducing carbon dioxide will enhance the oxygen-binding capacity of hemoglobin.
And this is what carbonic anhydrase ultimately does – it reduces carbon dioxide by transforming it into bicarbonate and protons.
Carbonic anhydrase 9 can be induced within minutes. But its degradation would likely depend on protein turnover rates.
For this reason, night-time bouts of hypoxia could induce changes lasting for days.
And this may tend towards reduced cerebral blood flow because of high expression of carbonic anhydrase, lowering the protective and vasodilatory CO2.
Reduced cerebral blood flow is a classic finding in dementia – reported about as often as low acetylcholine, if not more so.
“Perfusion deficits were detected in 34 of 35 patients but in only 4 of 35 controls.” (O’Brien)
Magnesium increases blood flow to the brain…
And perhaps that’s why it’s been successfully used to treat dementia.
Yet, regardless of the primary mechanism behind hypoxia and dementia, there is enough published evidence to conclude that it’s causal.
So “undercover sleeping” is probably not something to make a habit of…
And if “undercover sleeping” is already a habit, care should be taken in choosing the right blankets.
“Among older women, sleep-disordered breathing was associated with an increased risk of developing cognitive impairment 5 years later. In addition, even after adjusting for demographic risk factors and comorbidities, we found that 2 of 3 indices of hypoxia (but not sleep fragmentation or duration) were associated with incident mild cognitive impairment or dementia, suggesting that hypoxia is a likely mechanism through which sleep-disordered breathing increases risk for cognitive impairment.” (Yaffe, 2011)
—-Important Message for Men Worried About Effects on Penile Health—
7 minute method brings more oxygen-rich blood flow to the member (brings erections back)
You may be breathing in a lot of air — but what counts is how much oxygen actually reaches your penile tissues, your prostate, and your testicles…
And how does oxygen reach the male member? Through blood flow.
Men need lots of oxygen-rich blood flowing to their members to get big, thick, and engorged boners.
So I started coming up with a protocol that could reverse tissue hypoxia and bring men even more oxygen “down there”…
And I’m proud to say it works… in as little as 7 minutes…
I call it the Oxygenate Your Penis protocol, and it doubles the amount of oxygen-rich blood flowing through a man’s penile chambers.
———-
