This new study, which I can’t believe came out of the United States, has me completely amazed. The crushing powers of Big Pharma here tend to suppress this kind of breaking research.
Type 1 diabetics are achieving complete insulin independence with this new technique.
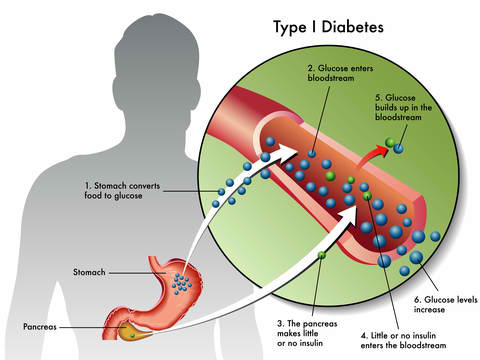
Type 1 diabetes is tough. It’s when your insulin producing cells have been mistakenly destroyed by the immune system. And for most people it means managing their blood sugar through daily doses of insulin.
The pharmaceutical companies love this, of course. It just means more money in their pockets – especially since they’ve been jacking up the price of insulin over the last 20 years or so.
But this new technique offers a great deal of hope (there are also some very positive things you can do with your diet to feel way better – more on that later) for Type 1 diabetics.
Pancreatic islet cells transplanted within a tissue-engineered platform can successfully engraft and achieve insulin independence in Type 1 diabetics.
Not a new technique, but a new way of doing it
This technique called “islet implantation” isn’t new, but there have been some problems with it up till now, even though it’s gotten good results.
Some patients who have received islet transplants at the DRI have been insulin independent for more than a decade, as DRI researchers have published.
The problem with it is that the cells that produce the insulin called “islets” used to be implanted in the liver, which produces a big-time inflammatory response and potential rejection.
The inflammatory reaction that is normally observed when islets are implanted in the liver or in other sites with immediate contact to blood.
This kind of response is bad news for the body, where any inflammation can cause cascading health problems. And so this application of islet cells to the liver, even though it works, has been very limited until now because the islets that replace the insulin production can’t really come into contact with blood and there has been no other way to implant them.
It all starts in the gut to create a so called “mini pancreas”
I’m a HUGE believer in gut health because it contributes to overall health in major, major ways. But this is something a bit different.
This involves a body part you may have never heard of (I don’t think it’s talked about much in health class for sure).
It’s called the omentum.
Which is an apron like tissue that covers the abdominal organs.
The big advantage of putting the insulin producing islets into the omentum instead of the liver to this is that eventually it could replace the functioning of the pancreas without the need for anti-rejection drugs and without the inflammatory response associated with placing these islets in the liver.
So type 1 diabetics may eventually have a real solution to insulin dependence that actually works.
“The objective of testing this novel tissue-engineered platform is to initially determine that insulin-producing cells can function in this new site, and subsequently introduce additional technologies towards our ultimate goal to replace the pancreatic endocrine function lost in type 1 diabetes without the need for anti-rejection drugs, what we call the DRI BioHub,”
This is amazing, but it’s not there yet. You’ll notice that in the study they say “ultimate goal”. Which means that anti-rejection drugs are still necessary and it’s still in the trial phases. So unless you are lucky enough to get into a trial, this therapy isn’t likely to be available for quite some time.
But still, the idea that science will be able to implant these islets and have your body produce its own insulin again is mind-blowing.
So if you have type 1 diabetes is there any other hope?
Avoid This Type of Fat to help with Metabolism and Inflammation
Up until about the 1950s most people ate animal fat. Things like lard and butter.
Then there was this health push (sponsored by Big Ag by the way) to get people to eat poly-unsaturated fats, instead of saturated fats, because they were supposedly healthier. It’s what I’ve been told my whole life and probably what you’ve been told too.
But these kinds of fats – things like vegetable oils, soy oil, fish oil, and canola oil all have serious health consequences, because they produce major inflammation in the body and depress the metabolism.
A lot of times people with Type 1 diabetes think it’s the diabetes that is causing the weight gain and tiredness, but often it’s the PUFAs.
Omega 3 and Omega 6 fatty acids (PUFAs) are extremely unstable. If you leave them out they turn into a disgusting, sticky mess.
And that is exactly what they do in your body as well.
They gum up the works. And make you feel like crud.
Now I know there are tons of studies that show the benefits of things like fish oil, but these are all done short term, so the long term effects aren’t shown often.
But you need to know about them.
Because the evidence for consuming Fish oil and other types of PUFAs in quantities is just not their.
So if you have diabetes (Type 1 or Type 2) and are struggling with weight gain or tiredness, try eliminating the PUFAs for about 6 months. Watch out for PUFAs in processed foods like crackers and potato chips, because they hide EVERYWHERE.
And instead of PUFAs eat coconut oil and butter in small amounts. These fats are very stable both on the shelf and in the body.
The results may very well amaze you. Many people report losing weight with much less effort and feeling less achy.
Because if you can’t get into one of these amazing trials, you might as well start feeling better and better by taking care of your metabolism and inflammation responses. For more in depth health advice, sign up to our daily newsletter. You will be blown away.
Citations:
http://www.nejm.org/doi/10.1056/NEJMc1613959
