
Finally, a solution to my embarrassing “shrinkage” problem…
—-Important Message—-
Why has my penis shrunk?

My shrinkage caused a problem for me and Jodi in the bedroom…
It was absolutely dreadful. I was always so worried about her noticing me getting smaller “down there…”
So finally, I built up the courage to actually talk to her about it shrinking, and she told me she HAD noticed it…
The worst thing you want to hear as a man… but I did not give up…
I discovered a way to naturally get my size back and stop shrinkage altogether — and it also gave me a boost in performance!
Here’s what I’m using to make my member grow in size and stamina.
———-
Why you must fix your constipation
If you aren’t having two or three good healthy bowel movements a day, you need to read today’s newsletter.
But a superficial analysis of the role of serotonin in constipation is likely to lead to confusion…
There are many apparent paradoxes involved and seemingly contradictory data.
For instance…
Increases of serotonin have been reported in the colons of constipated subjects multiple times…
Yet serotonin consistently induces diarrhea when either ingested or injected.
Serotonin always stimulates the small intestine when applied directly…
But it also paralyzes the colon.
“The original name for serotonin (5-hydroxytryptamine; 5-HT) was enteramine because it was initially discovered in the gastrointestinal tract, and the gut is the major source of 5-HT in vertebrates.” (Costedio, 2009)
Some serotonin receptors induce muscle contraction (5-HT1, 5-HT2A, 5-HTA3)…
While others, ostensibly the auto-feedback ones, have been shown to do the opposite (5-HT4, 5-HT7).
Opiates decrease motility (our ability to move food through the digestive tract) and serotonin increases it…
But, paradoxically, morphine (an opiate) has been shown to release serotonin.
Yet, despite these apparent contradictions, serotonin’s function in the intestinal tract ultimately makes sense.
Serotonin seems to be synthesized and stored by enterochromaffin cells (EC cells) as a diarrhea-causing agent to be used in times of infection and irritation.
(EC cells are in the lining of the digestive tract and play a crucial role in gastrointestinal regulation.)
The perennial mainstream theory frames serotonin’s involvement as necessary for peristalsis (digestive food releases serotonin which subsequently stimulates waves of motion that move the food along).
But this has been proven false many times over…
Animals depleted of intestinal serotonin have normal peristalsis.
And even though morphine has been shown to release serotonin and stimulate intestinal contractions, these effects are invariably non-propagating and non-propulsive. (They don’t move anything along.)
Intestinal opiate receptors are exclusively found on circular muscle cells and are absent on longitudinal muscle cells, or those which propagate motility waves.
Small amounts of serotonin on intestinal circular muscles could cause a clamping effect.
But larger amounts, such as occurs after EC cell degranulation, effectively spill over to the longitudinal muscle and induce motility via those.
“The largest known stores of serotonin are in the enterochromaffin cells of the jejunum. Serotonin is released by the small intestine in response to distention and intraluminal hypertonic solutions.” (Johnson, 1962)
Opiates also inhibit the release of acetylcholine and epinephrine (neurotransmitters).
Although serotonin is commonly increased in the colon of constipated patients this finding isn’t universal.
(Serotonin contents of distal and sigmoid colons are the only ones reported – on account of accessibility – so little can be said about serotonin in the small intestine.)
Enterochromaffin cells (EC cells) can degranulate and release the majority of their contained serotonin.
So finding increases in constipated subjects where there’s less output shouldn’t be very surprising…
Degranulated EC cells take time to refill their serotonin stores.
So even though serotonin’s role may initially seem confusing, this is mainly due to the failure to discriminate between circular and longitudinal muscles.
It could also be due to not appreciating the fact that serotonin that is not released is stored, and thus may accumulate.
Here’s some evidence that serotonin’s presence in the GI tract is primarily to serve as a diarrhea-causing agent and isn’t necessary for normal motility:

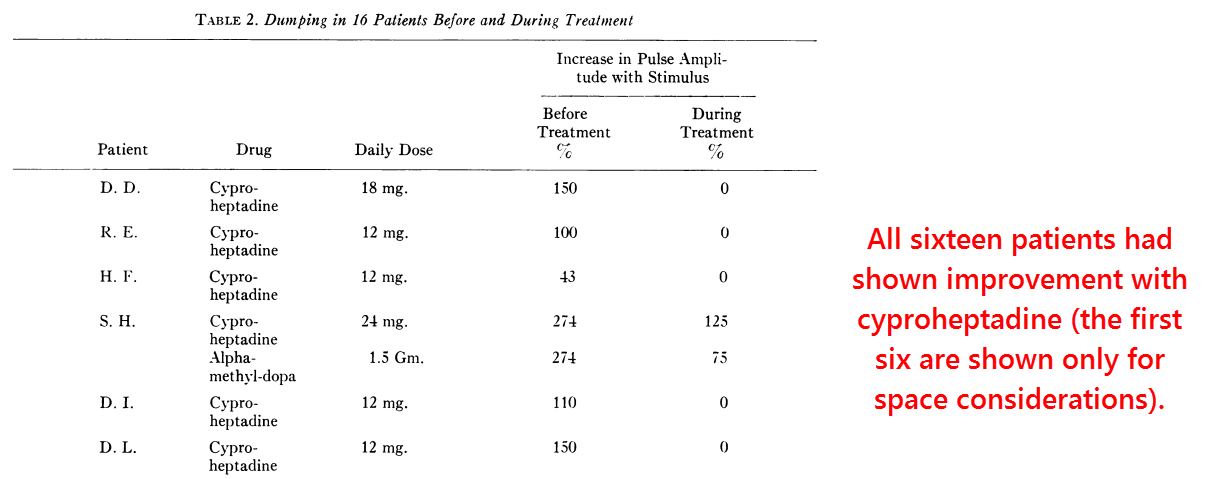
This article is about the “dumping syndrome” – an anomaly characterized by a reduction in blood pressure and diarrhea shortly after a meal.
This usually occurs in people who’ve had a gastrectomy, and happens when partially-digested food stimulates the release of serotonin from EC cells.
This effect can be induced experimentally by hypertonic solutions of salts and sugars – in this study it was 50% glucose – that have been shown to degranulate EC cells and release serotonin.
The reduction in blood pressure is likely a consequence of fluid moving out of the blood and into the intestines.
And, predictably, the 50% glucose solution induced the “dumping syndrome” in all of these patients:

Yet more importantly: These experimenters found that serotonin antagonists would inhibit this response.
This occurred both in human patients and in dogs (which had also been administered 50% glucose solution, but straight into the duodenum, not the gastrectomized stomach).
Anti-serotonin drugs effectively reduced diarrhea and led to weight gains in most subjects.
Cyproheptadine, reserpine, and alpha-methyl-DOPA were all effective in this study.
The idea that enterochromaffin cells (EC cells) are being depleted in patients with “dumping syndrome” is also suggested by reports of them being free of symptoms shortly following each episode…
And after that, serotonin stores re-accumulate and restart the cycle.
EC cells synthesize serotonin from dietary tryptophan.
“Shortly after a dumping episode with release of available serotonin, the patient may find he can eat with only minimal symptoms or none at all. However, with re-accumulation of serotonin stores during an overnight fast, the patient frequently finds his most severe symptoms occur after breakfast.” (Johnson, 1962)
That fact that EC cells can degranulate and release the majority of their stored serotonin has been determined histologically.
As a fluorescent molecule, serotonin can be visualized by tuning out certain wavelengths of light using filters.
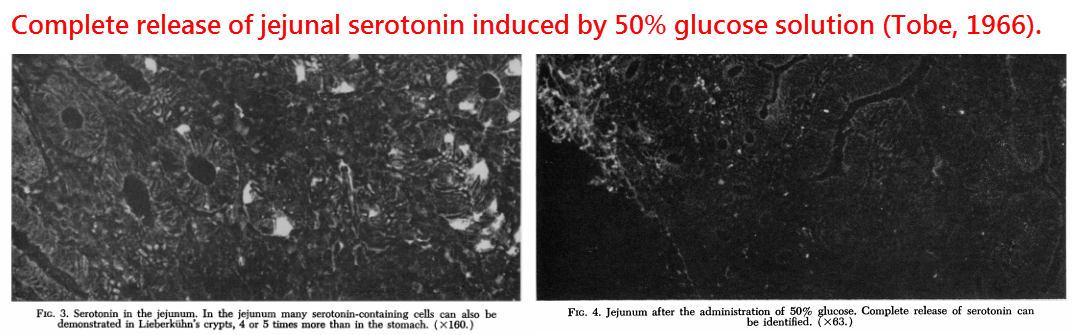
Besides hypertonic solutions of magnesium sulfate and/or glucose, which literally swell the cells until they explode, serotonin can also be released by strong acid.
This latter effect is likely mediated through acid-sensing TRPA1 ion channels.
Highlighting the immuno-responsive role of EC cells is the fact that they can be degranulated by LPS (lipopolysaccharide or endotoxin), interleukin-1-beta (a cytokine), and cholera endotoxin.
Entamoeba histolytica (a parasitic infection) also induces diarrhea.
It doesn’t do this via an endotoxin, though. It does it by synthesizing enough serotonin to do so directly.
Either way, the response can be effectively blocked by bufotenine – an anti-serotonergic drug:

This is the same bufotenine that can be found in toad skin and certain species of psychedelic mushroom.
Hypertonic solutions can provoke so much cell degranulation that serotonin can, in fact, be detected in the portal vein.
The portal vein runs from the intestine to the liver, after which the serotonin is largely degraded by the enzymes monoamine oxygenase and indoleamine dioxygenase.

Since EC cells reliably degranulate after contact with LPS and cholera toxin, then at least one of their functions is to initiate diarrhea in times of infection.
Yet there’s also evidence that this could be their only role, with the mechano-transduction theory being little more than wishful thinking.
This is evidenced by serotonin-depleted rats having normal motility:
In this study, they used two groups of rats, one group fed a tryptophan-free diet and another group fed an identical diet but with added L-tryptophan (0.4%).
This technique was quite effective, and led to nearly complete serotonin reductions after one month… Two animals had no detectable serotonin in their intestines.
They also gave some rats reserpine to deplete serotonin, yet tryptophan deprivation alone was just as effective:
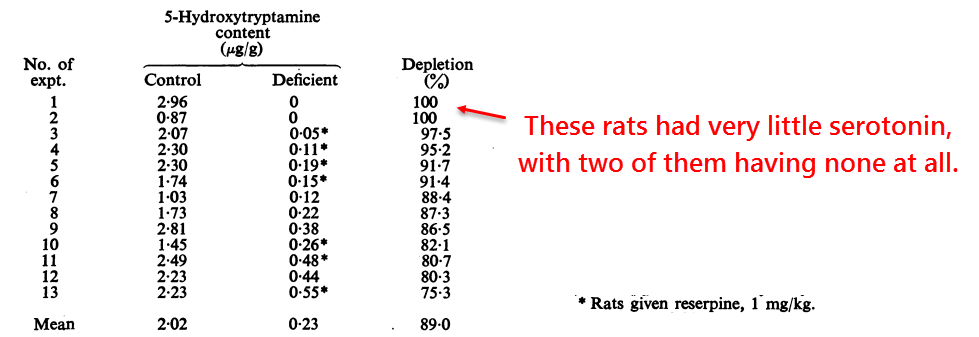
Then they measured peristalsis by anesthetizing the rats and measuring pressure waves after administering a liquid.
They also recorded longitudinal muscle contraction and the volume of fluid expelled.
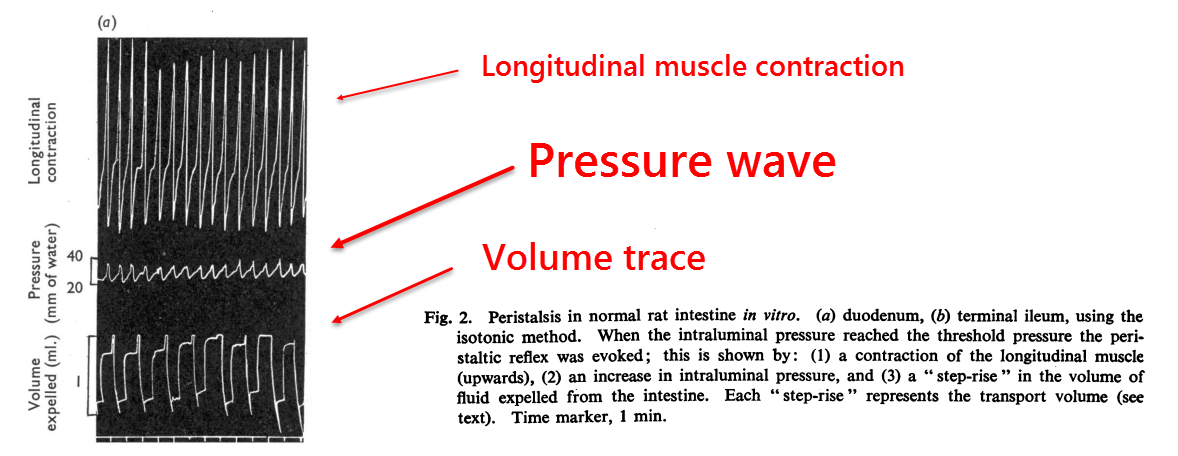
And they found essentially no change whatsoever in serotonin-depleted rats.
This study confirmed a previous serotonin-depletion study that had used reserpine (Bülbring, 1959).
But this study did so more reliably as they also used tryptophan restriction.
“Whatever the precise location of sensory receptors which trigger peristalsis, the present experiments strongly suggest that 5-hydroxytryptamine (serotonin) is not obligatory as a sensory stimulant or essential for peristalsis in any way.” (Boullin, 1963)
This study should have forever killed the mechano-transduction theory…the theory that states that the serotonin released by objects in the intestine is needed to propel them.
But it didn’t. And this idea still persists.
These experimenters also observed the animals throughout the entire month of serotonin depletion without noticing any changes in elimination.
So, not only did these rats demonstrate normal peristalsis in the absence of serotonin, they also showed normal elimination in the weeks leading up to the recording of results.
“More critical is the evidence which showed that peristalsis (in vitro and in situ), was normal in tryptophan-deficient rats before any 5-hydroxytryptamine (serotonin) had been given.” (Boullin, 1963)
This experiment could perhaps be disregarded as outdated because it is over 50 years old…
But there is newer evidence showing the same.
Using genetic engineering to construct serotonin-free rodents, investigators from Columbia University had recently confirmed these results (Li, 2011).
They showed that mice lacking tryptophan hydroxylase-1 (TPH-1) had normal motility despite having no serotonin in enterochromaffin (EC) cells.
TPH-1 regulates serotonin synthesis in the periphery, including EC cells, and tryptophan hydroxylase-2 (TPH-2) creates it for the nerves and brain.
Yet since tryptophan is the sole precursor of serotonin, you’d expect the rats in the Boullin study (above) to lack serotonin everywhere.
Despite this, Boullin’s animals demonstrated normal peristalsis in every way.
“The results indicate that its presence is not obligatory, though the amine may have an ancillary, physiological effect, both on the peristaltic reflex itself and on the movements of the pyloric sphincter.” (Boullin, 1963)
Peristalsis is more fundamentally controlled by acetylcholine, not serotonin.
And that is evidenced by the side effects of cholinesterase inhibitors.
This fact makes lobeline doubly effective because, besides being a natural anti-opiate, it is also a cholinergic agent.
So gut serotonin appears to exist as an emergency evacuation molecule and can thus explain IBS-D and IBS-M, but not IBS-C.
Opiates and methane better explain constipation.
The only intestinal muscles that serotonin inhibits are found in the distal colon, an area representing only a small fraction of the total length of the colon.
Assuming serotonin is an emergency evacuation molecule, this effect could be desirable – thus preventing a constant outflow.
So it’s possible to use an anti-serotonin treatment without apprehension, as the molecule it is inhibiting doesn’t appear to be necessary.
Serotonin doesn’t seem to be entirely necessary for anything, and methods employed to antagonize serotonin generally lead to enhanced focus and attention.
“Cyproheptadine is a potent serotonin antagonist equivalent in activity to lysergic acid diethylamide in its ability to inhibit the response of tissues and organs to serotonin.” (Johnson, 1962)
—-Important Message—-
Hair loss may be reversed in men — here’s how

I’ve discovered a simple mixture of natural ingredients that oxygenates the hair follicles to improve blood flow…
And when more blood is flowing into the hair follicles, it promotes natural, new growth.
Suddenly you’re seeing less hair in the sink and more on the top of your head.
Just put this herbal balm on your scalp at night before bed, and let it work while you sleep.
I’m calling it my natural “Hair Secret” and you can have it for free.
———-
