
One of the best herbals or just hype? Here is the truth about berberine

—-Important Message From Our Sponsor—-
Here’s what happens when you send this text to your wife or girlfriend
I thought this guy was full of it when he told me he could turn on ANY woman just by TEXTING her…
Then I used it on MY wife…and all I can say is…
WOW! This really works.

And all it takes is a few thumb flicks…
Here’s what to text her — just copy and paste this
———-
Berberine and how to use it
Of all the treatments used to treat blood sugar problems, there’s perhaps none with a greater reputation than berberine. And this is for good reason.
Originally isolated from the roots of Coptis chinensis, it’s antidiabetic utility was recorded as early as 510 AD in the ancient text called Miscellaneous Records of Famous Physicians.
Although its antidiabetic effect was not rediscovered until recently (Chen, 1986), its high degree of efficacy has since generated considerable notoriety.
For instance…
Just searching for “berberine and blood sugar” on Google Scholar yields 23,300 results…
That would imply that it’s been studied more than phlorizin and naringenin in this capacity.
This search result is second only to metformin and ginseng among natural antidiabetic compounds.
Enough research has now been done on berberine to know what it does, how it does it, and what dose provides the best antidiabetic effects.
But, before we examine its mechanisms and biological targets, just have a look at how effective it really is:
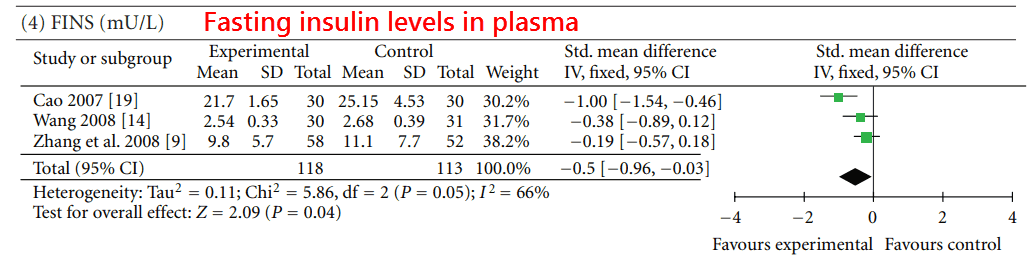
The authors of this meta‑analysis sifted through all the randomized clinical trials they could find…
Eventually they selected the larger ones that were also similar enough to each other to be compared.
They settled on 14 trials involving 1,068 participants, all including a dose range of 500-1,500 mg of berberine per day.
They compared the data in many ways…
But perhaps the most relevant comparison was “berberine with lifestyle modification” versus “placebo with lifestyle modification.”
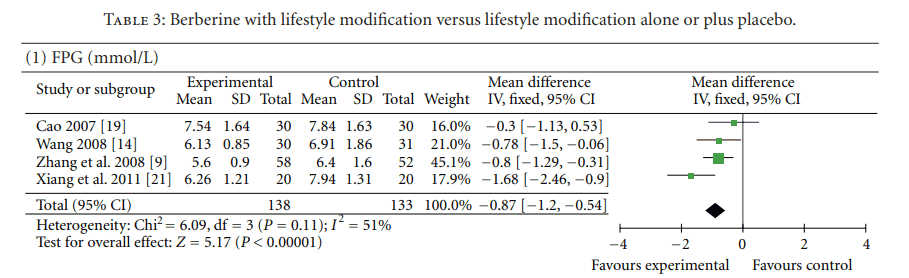
As we can see above, the fasting plasma glucose (FPG) was significantly lower in the berberine group.
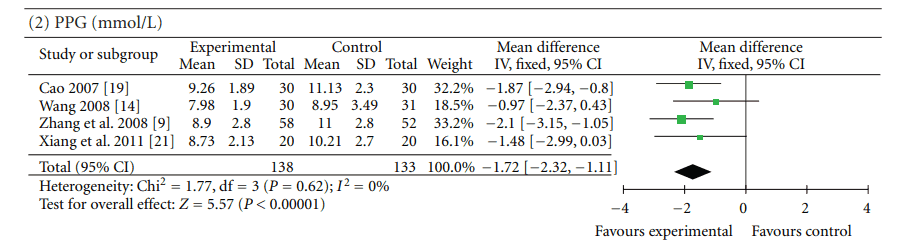
Postprandial plasma glucose (PPG) was similarly lower in the berberine group, as seen below. And fasting insulin concentrations (FINS) were as well.
This “insulin-sensitizing effect” of berberine was noted by others (Ko, 2005), and does give insight as to how it works.
Berberine obviously doesn’t work through simply “increasing insulin” as sulfonylureas do.
But it either acts to enhance the effect of insulin or to lower glucose in some other way.
(With less glucose in the plasma, less insulin is needed.)
Experiments show that the former is the case – or that less insulin is needed for glucose uptake in the presence of berberine:
This researcher first examined the ability of extracts from Coptidis rhizoma (Huang Lian – a root used in traditional Chinese medicine) to enhance glucose uptake…
And he confirmed that it corresponds perfectly to the berberine content of the extract.
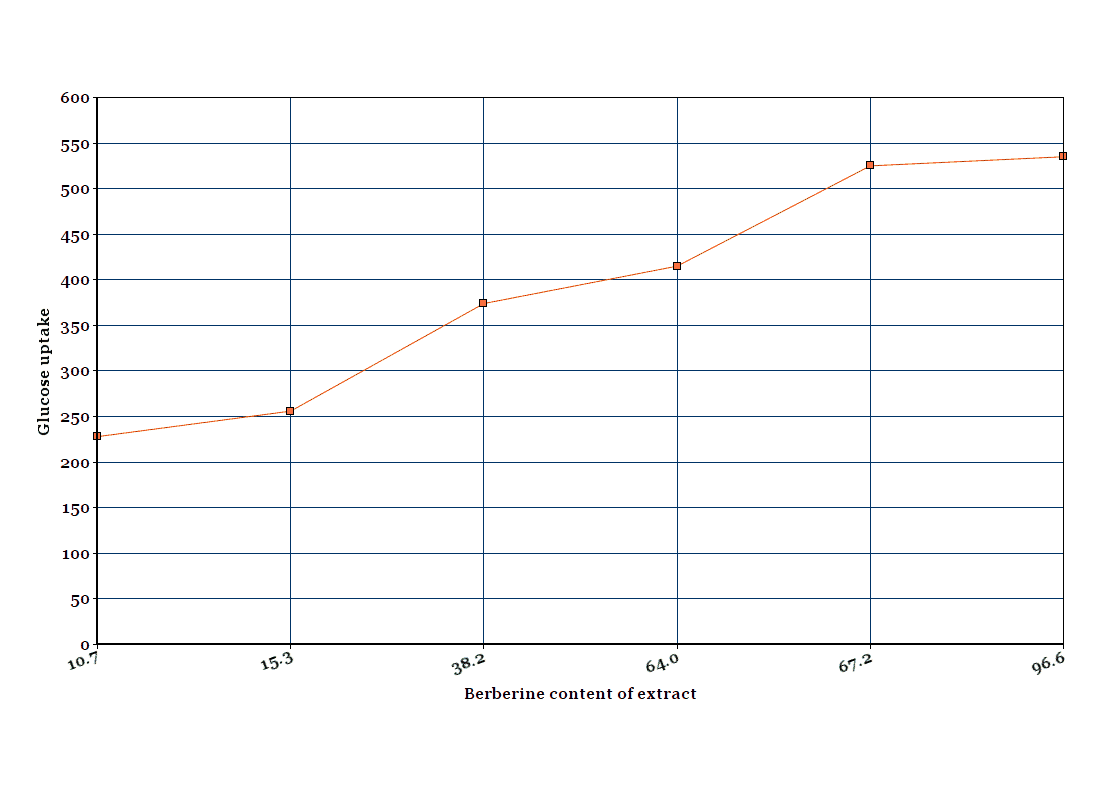
He presented his data in table form only, but I’ve depicted the same values as a line graph below:Then he compared berberine against the blood sugar treatment called pioglitazone – a PPARγ (peroxisome proliferator-activated receptor) agonist.
And he also compared berberine against exendin‑4, a stable analogue of glucagon‑like peptide that promotes insulin secretion.
He wanted to check their relative abilities (berberine versus the other two things) to stimulate glucose uptake.
He found that all three of these compounds (including berberine) stimulate glucose uptake – but only in the presence of insulin.
This fact is important, as they’re only amplifying physiological signals already in place – NOT creating entirely new ones.
We all know that excess insulin, when released or administered inappropriately, can lead to dangerous states of hypoglycemia.
And we only need enhanced glucose uptake in certain instances, such as right after eating.
“However, most of them stimulate insulin secretion with and without glucose challenge… As a result, they increase insulin secretion without glucose loading, resulting in exhausting and damaging beta-cells and frequent hypoglycemia… Thus, an insulinotropic agent is a better anti-diabetic agent than a simple insulin secretagogue.”
And berberine was potent in doing this – with only 5 μM working similar to 2 μM of pioglitazone (and without the accumulation of triglycerides).
This means that berberine doesn’t work through activating PPARγ.
It also means that it does something with the glucose besides converting it into lipids.
In fact, newer studies have shown that berberine activates glycolysis.
And perhaps that reveals the fate of the increased cellular glucose.
Berberine is also safer than thiazolidinediones (another diabetes medication).
And it is more affordable – and available without a prescription.
Actually, both berberine and exendin‑4 decreased triglyceride accumulation…
And that means that the way it works is more similar to glucagon‑like peptides than endogenous PPARγ ligands (e.g. prostaglandin J2 or serotonin metabolites).
He also extracted and separated certain glucose‑related proteins – such as IRS‑1 (insulin receptor substrate 1) and GLUT‑4 (glucose transporter type 4) – from the cells to look for changes.
Such changes could help us infer its mechanism of action.
He found increases in phosphorylated IRS‑1, the active form of the insulin receptor substrate, and also the cell membrane glucose transporter GLUT‑4.
IRS‑1 is directly activated by the insulin receptor.
Scientists assume it is responsible for mediating the entire signal thereafter.
In fact, insulin is entirely ineffective without this peptide.
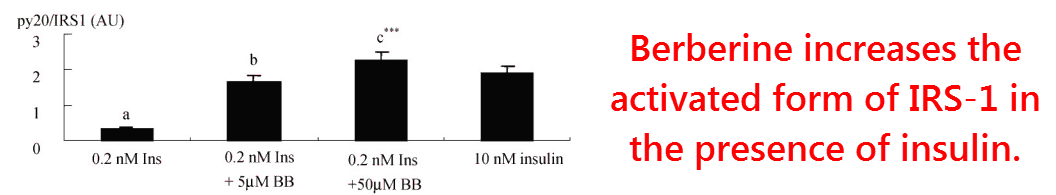
Just 5μM of berberine increased the activated form of IRS‑1 caused by .2 nM of insulin up to that induced by 10 nM of insulin.
This is huge… And it explains the reduced need for insulin observed in clinical trials.
So how does berberine do this?
The increases he noted in GLUT‑4 and activated IRS‑1 are just effects…
So that doesn’t say anything about berberine’s initial target.
Yet, fortunately, berberine’s molecular target was discovered just one year later by researchers at the University of Jordan:
Upon reading experimental evidence about berberine, these researchers surmised that maybe it works by inhibiting protein tyrosine phosphatase (PTP‑1B).
PTP‑1B is an enzyme.
It is responsible for inactivating the insulin receptor and the epidermal growth factor receptor after internalization.
This enzyme (PTP‑1B) also inactivates IRS‑1.
Mice genetically engineered to lack PTP‑1B have enhanced insulin sensitivity and a higher concentration of activated IRS‑1.
They are also immune to the weight gain caused by a high‑lard diet.
Inhibitors of PTP‑1B are a recognized class of antidiabetic agents.

These researchers used molecular computing to estimate how well berberine should bind to PTP‑1B…
More importantly, they also assayed its activity on the actual enzyme as well.
Using a peptide from the epidermal growth factor receptor as substrate, they found that berberine could inhibit PTP‑1B in nanomolar concentrations.
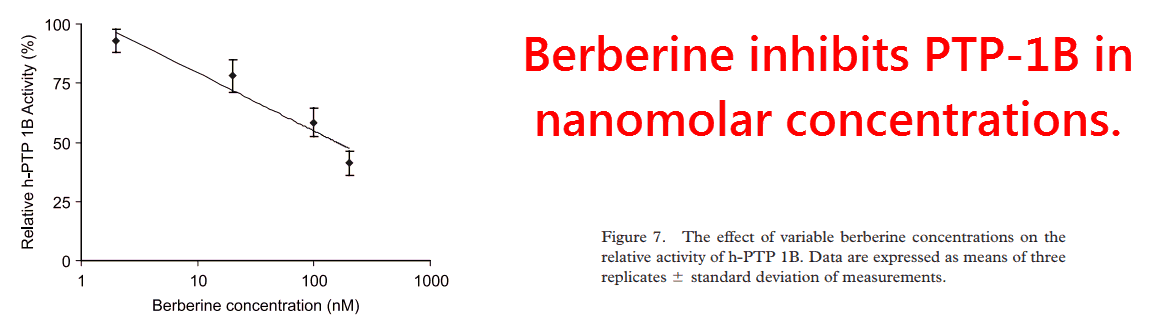
This is certainly the most potent activity discovered so far for berberine.
In addition, it is essentially the only one of significance – considering its low bioavailability and effective dose.
The ability of berberine to inhibit PTP‑1B was confirmed four years later (Chen, 2010).
Yet berberine has also been shown to inhibit dipeptidyl peptidase‑IV (DPP4).
DPP4 is an enzyme expressed on the surface of most cell types.
Among other functions, DPP4 is associated with immune regulation, signal transduction, and apoptosis (cell death).
Berberine does this to DPP4 with an IC50 (that’s kind of a half-life) of 13.3 μM.
Even though this is 84 times higher than its activity on PTP‑1B, higher oral doses could result in intestinal concentrations needed to inhibit this enzyme…
DPP4 is highly expressed in the small intestine.
It is responsible for rapidly degrading glucagon-like peptide (GLP‑1), a signaling hormone that also increases insulin sensitivity.
For this reason, DPP4 inhibitors are also a recognized class of antidiabetic compounds.
Inhibition of DPP4 is likely why berberine increases GLP‑1 when higher doses are given orally:
This study used human intestinal L‑cells to measure GLP‑1 release under various berberine concentrations.
They found some effect, but only at the higher doses.
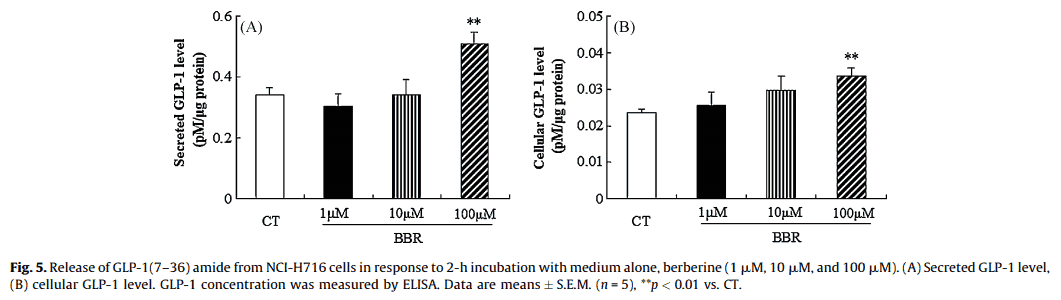
Yet they found a greater response in living rats, perhaps because the majority of DPP4 exists in the capillaries leading from intestinal L‑cells to the pancreas.
Berberine most likely increases GLP‑1 by inhibiting this enzyme…
So you would expect to see more response when there’s more enzyme to inhibit.
This could explain why a higher (120 mg⁄kg) dose of berberine per day, when fed to rats, can cause a significant increase of GLP‑1 in the portal vein after a meal:
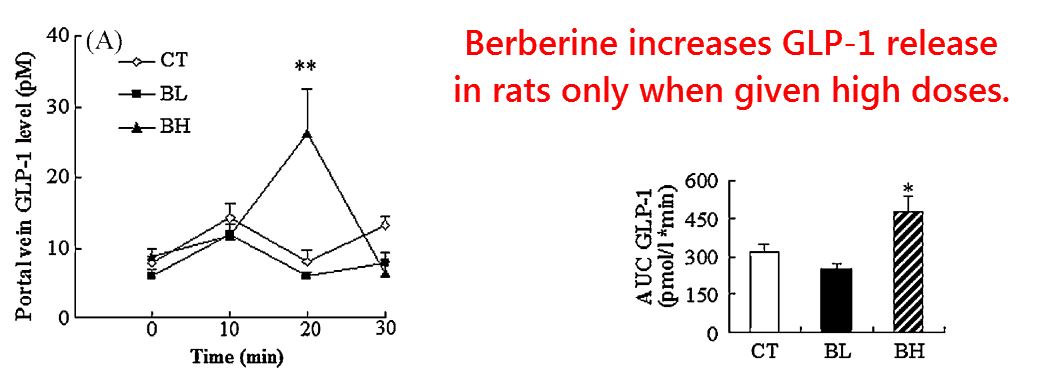
Why this did not occur in the 60 mg⁄kg berberine group could be explained by the drug’s somewhat low bioavailability and moderate potency.
When translated into the human equivalent dose (HEC), the low‑berberine group consumed basically 9.68 mg⁄kg per day.
The low dose, in turn, corresponds to 677 mg per day for a 70 kg human, or approximately the average dose used in clinical trials.
And the high‑berberine group would correspond to twice these values – a human dose of 1,355 mg per day.
So, in essence, both antidiabetic effects of berberine are achievable at normal doses.
The insulin‑sensitizing effect achieved through inhibition of PTP‑1B at lower doses becomes potentiated by GLP‑1 at higher doses.
“Thus, herbs or drugs for type 2 diabetes mellitus should have an insulin-sensitizing action to relieve insulin resistance and an insulinotropic action to improve glucose-stimulated insulin secretion and pancreatic beta-cell survival.”
Glucagon‑like peptide (GLP‑1) has insulin‑sensitizing activity in itself.
But it is so rapidly degraded by DPP4 that its main effect appears to be releasing insulin.
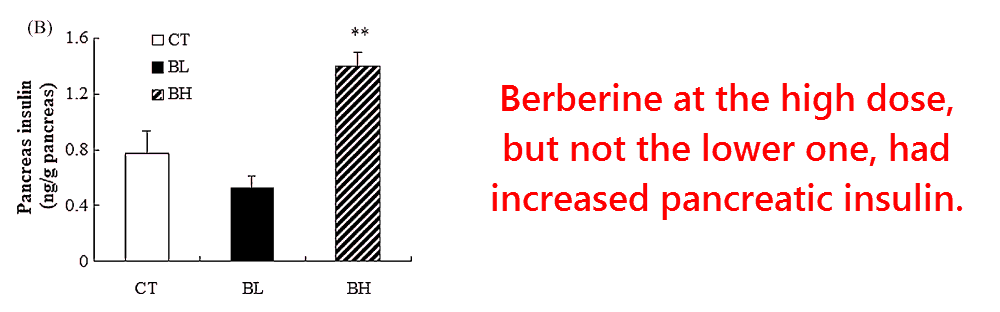
This study indeed implied that, as pancreatic insulin concentrations measured 30 minutes after glucose intake reflected those observed in GLP‑1.
Yet releasing GLP‑1 cannot be the only effect of berberine, as berberine has been consistently shown to stimulate glucose uptake in cell cultures without GLP-1 being present.
And also, the dose size generally taken by humans leads to a reduction of insulin – as less is needed (Dong, 2012):
So berberine is a combined PTP‑1B and DPP4 inhibitor…
This gives it the unusual distinction of belonging to two separate classes of antidiabetic compounds.
And that explains its high efficacy consistently reported in clinical trials – and also why it is the third most popular natural agent for blood sugar problems.
—-Important Message for Prediabetic and Diabetic Men—-
Why are so many doctors suffering from blood sugar problems
Diabetes has been skyrocketing amongst the entire population, even amongst physicians.
Why?
Maybe it’s because today’s diabetes treatments actually CAUSE diabetes to get worse and worse.
The answer is even MORE treatments, which makes it even worse…
Until diabetic men (and their doctors) are on six different “treatments” while they have nothing but a flat tire in the bedroom.
In fact, I do not know ANY diabetic men who are potent in the bedroom…
So, to avoid all that, I discovered a secret to reversing diabetes and it came from a strange place…
My dad.
———-
